An ocular foreign body occurs when an orbital foreign body penetrates into the globe itself, often threatening vision, and requiring urgent surgical removal.
Clinical presentation
Patients present in a highly variable manner based on the precise intraocular location and properties of the foreign body, as well as the presence of any additional trauma. Common symptoms include:
decreased visual acuity
photophobia
a "foreign body" sensation
Radiographic features
Imaging plays a crucial role in identifying an intraocular foreign body, particularly in the context of a hyphaema which limits clinical assessment of the posterior segment. CT is the modality of choice.
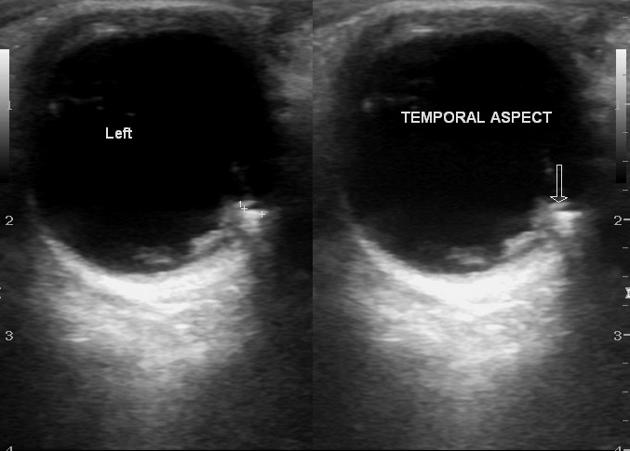
Ultrasound
Available at the point-of-care as a screening tool, many foreign bodies may be accurately identified with ocular ultrasound, however it is relatively contraindicated in penetrating injury. While sonographic findings differ based on the nature of the foreign body, common features include 2:
-
abnormal echogenic structure with posterior acoustic shadowing
may demonstrate a twinkling artifact on colour flow Doppler 1
reverberation artifacts are common
vitreous haemorrhage is commonly present
-
may demonstrate location-dependent mobility
a vitreous foreign body is more likely to be mobile than one in the posterior orbital fat
-
other associated injuries may include:
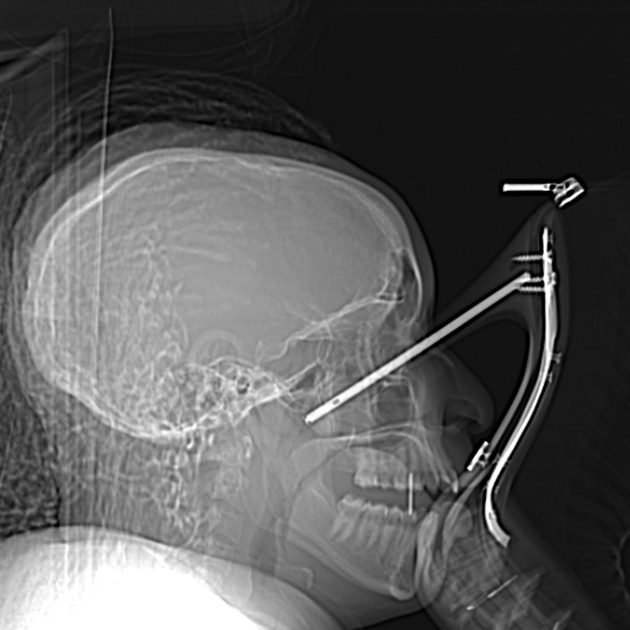
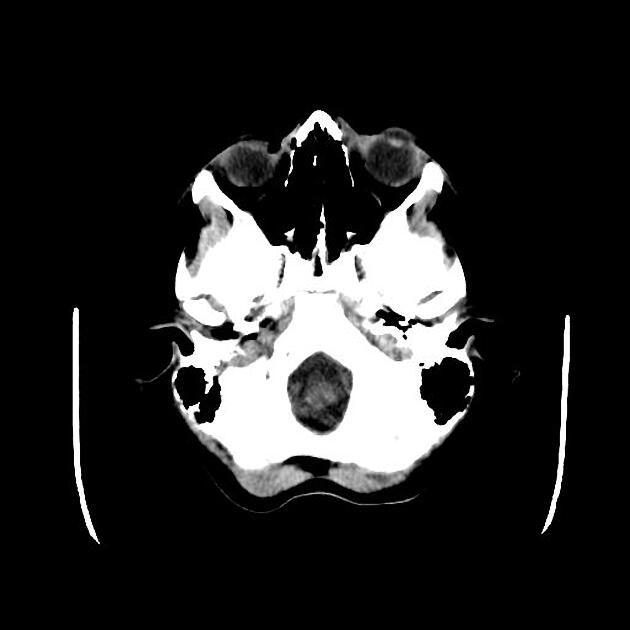
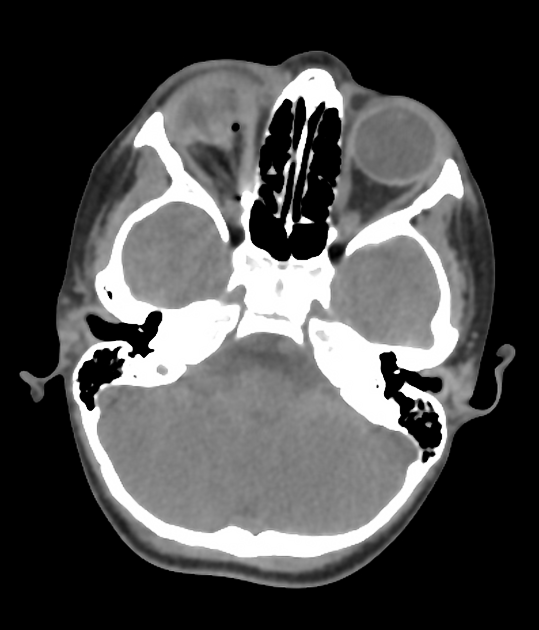
CT
A CT orbits is the examination of choice, as it provides superior localisation of small foreign bodies, the anatomy of the surrounding structures, and any associated injuries.
The density of the foreign body varies depending on the material. Metal is high density (>1000 HU) with associated beam hardening artifact. Glass is of variable density, ranging from 500-1900 HU. Wood varies with water content, with dry wood being as low as -600 HU.
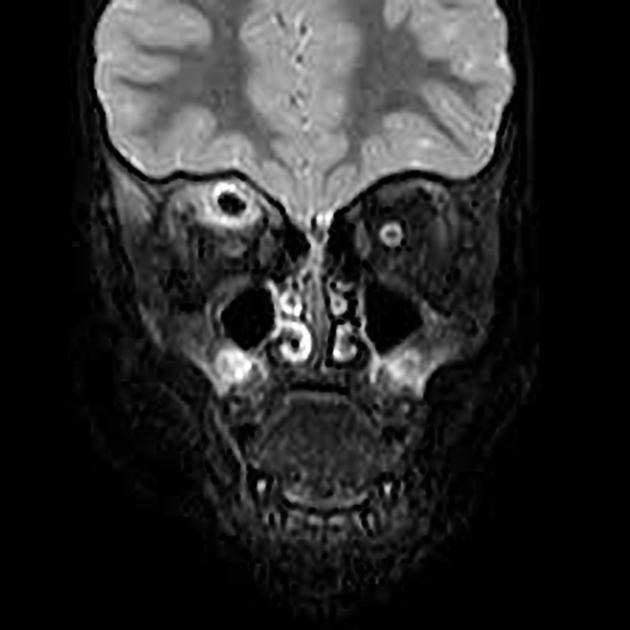
MRI
Rarely indicated in the acute context. MRI is contraindicated until metallic foreign bodies have been excluded with CT, x-ray or ultrasound.













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.