Germinal matrix haemorrhages, also known as periventricular-intraventricular haemorrhages (PVIH), are the commonest type of intracranial haemorrhage in neonates and are related to perinatal stress affecting the highly vascularised subependymal germinal matrix. The majority of cases occur in premature births within the first week of life. They are a cause of significant morbidity and mortality in this population.
On this page:
Epidemiology
Germinal matrix haemorrhage can only occur when the germinal matrix is present and is therefore only seen in premature infants. Haemorrhages can be identified in 67% of infants born prematurely at 28-32 weeks 1 and 80% of infants born between 23 and 24 weeks of gestation 2. The majority of haemorrhages (90%) are identified within 4 days of birth, and 40% within the first 5 hours 4.
Risk factors
Clinical presentation
Clinical presentation for grade I and II bleeds is vague. These are usually found on routine ultrasound performed on premature neonates. With grade III and IV bleeds, respiratory depression or apnoea, abnormal posturing, seizures, and bulging fontanelles may be seen 2.
Pathology
The germinal matrix is formed early during embryogenesis and is the site of glial and neuronal differentiation. From here cells migrate peripherally to form the brain. It is densely cellular and, not surprisingly, also densely vascular 2.
The blood vessels of the germinal matrix are weak-walled and predisposed to haemorrhage. Significant stress experienced by a premature infant after birth may cause these vessels to rupture. The bleeding occurs initially in the periventricular areas causing a periventricular haemorrhage (PVH). If this bleeding persists, the expanding volume of blood dissects into the adjacent lateral ventricles leading to intraventricular haemorrhage (IVH).
There is a direct relation between prematurity, germinal matrix and thus the number of capillaries in this region: at 32 weeks germinal matrix is only present at the caudothalamic groove. By 35-36 weeks gestation, the germinal matrix has essentially disappeared and thus the risk of haemorrhage is markedly reduced.
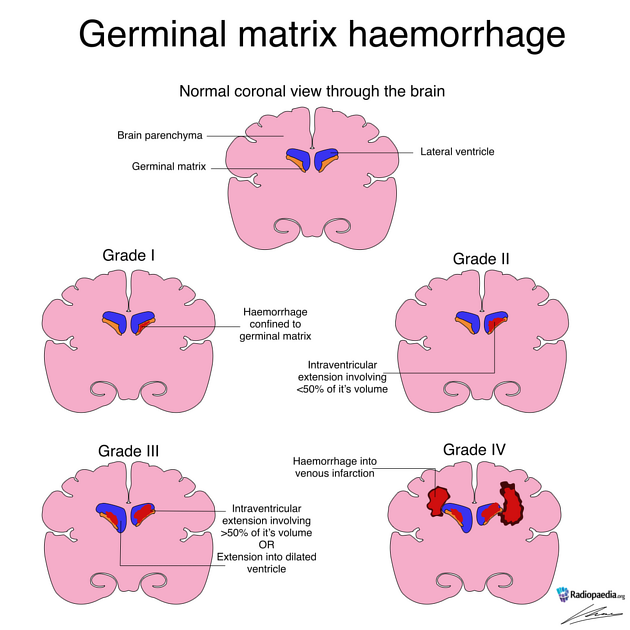
Classification
See: Grading of neonatal intracranial haemorrhage.
Radiographic features
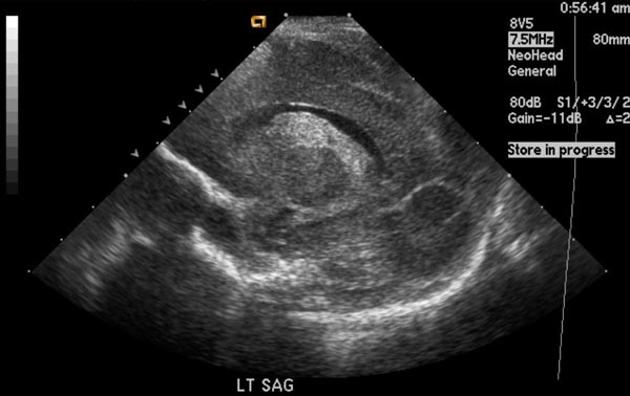
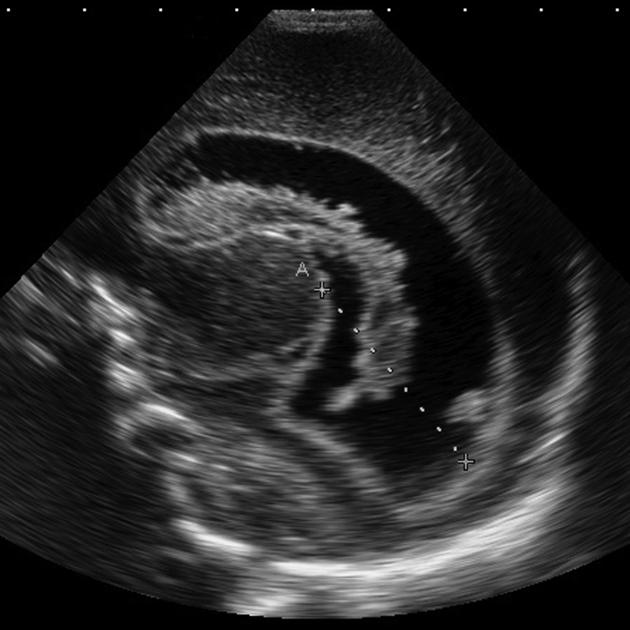
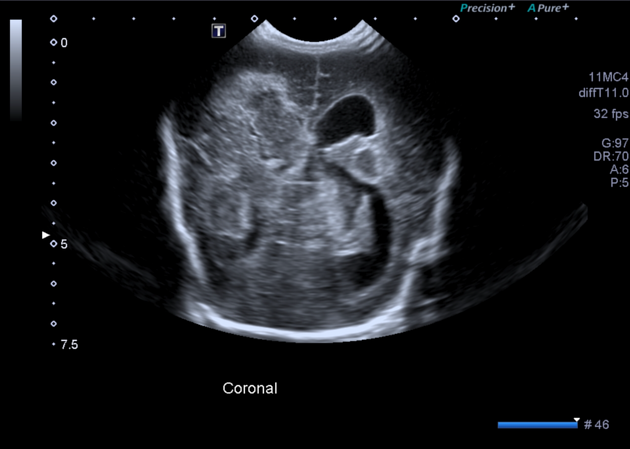
Ultrasound
This is the investigation of choice since it is portable and does not require sedation. Germinal matrix haemorrhages appear as echogenic regions close to the caudothalamic groove extending along the floor of the frontal horn of the lateral ventricle.
It is important to distinguish haemorrhage from the normal choroid plexus which is also echogenic. The caudothalamic groove acts as a convenient landmark: echogenicity anterior to the groove represents blood as the choroid finishes at the groove 4.
CT
CT may demonstrate high attenuating regions in keeping with haemorrhage which may or may not also be seen dependently within the ventricles.
With grade IV bleeds, large confluent regions of low density (venous infarction) and patchy regions of hyperdensity (haemorrhage) are seen in the periventricular regions. They are typically flame-shaped 4.
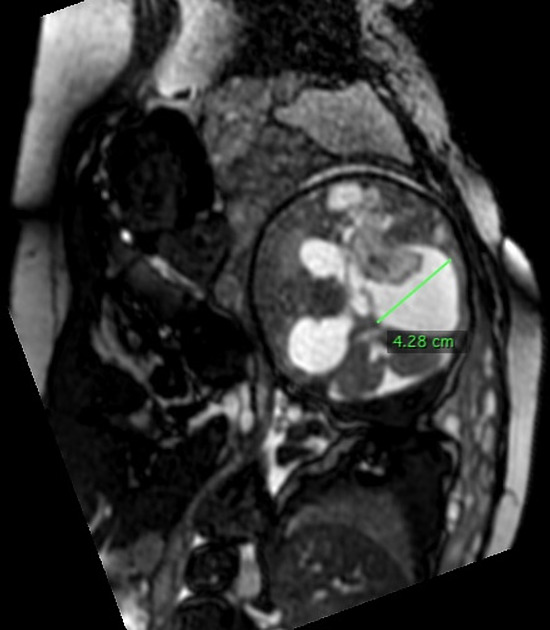
MRI
The appearance of the haemorrhage will vary according to the age of the bleed (see ageing blood on MRI).
Treatment and prognosis
The ideal treatment is the prevention of premature delivery. Antenatal dexamethasone administered to the mother or indometacin administered to the infant also decrease the incidence, although the exact mechanism by which this occurs is uncertain 2.
If hydrocephalus is present, CSF drainage may be necessary.
Prognosis depends on the extent of haemorrhage and the presence of hydrocephalus (see germinal matrix haemorrhage grading). Grade I and II haemorrhages have a good prognosis. Mortality rates are 3.1% (grade I), 7.8% (grade II), 21.3% (grade III), and 36.1% (grade IV) 5.
In grade IV bleeds, significant areas of cerebral tissue may be lost, forming porencephalic cysts.
Complications
post haemorrhagic hydrocephalus
blockage of villi
-
cyst formation
cavitation of haemorrhage
unilocular porencephalic cyst
Differential diagnosis
Differential considerations on antenatal ultrasound include:
normal choroid plexus: does not extend anteriorly to the caudothalamic groove/foramen of Monro
intraventricular haemorrhage of the newborn: within the subependymal region, rather than the germinal matrix
early periventricular leukomalacia: when echogenicity is increased, common in preterm
hypoxic-ischaemic brain injury: involves subcortical cerebral or basal ganglia injury; common in term babies
TORCH CNS infection: commonly seen with periventricular calcifications












 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.