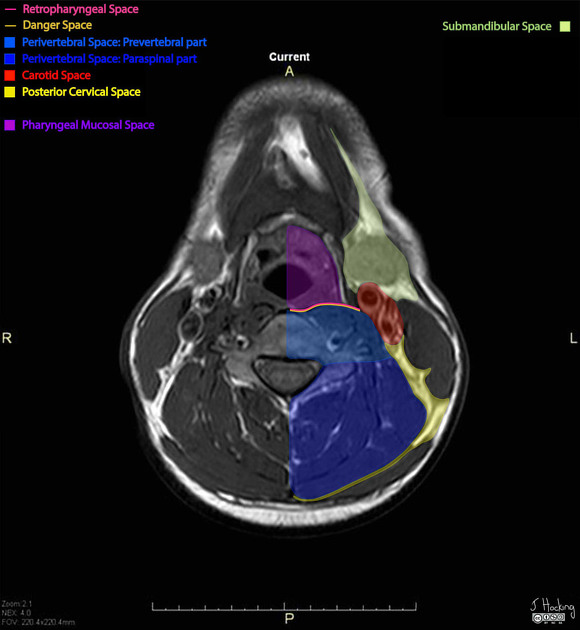
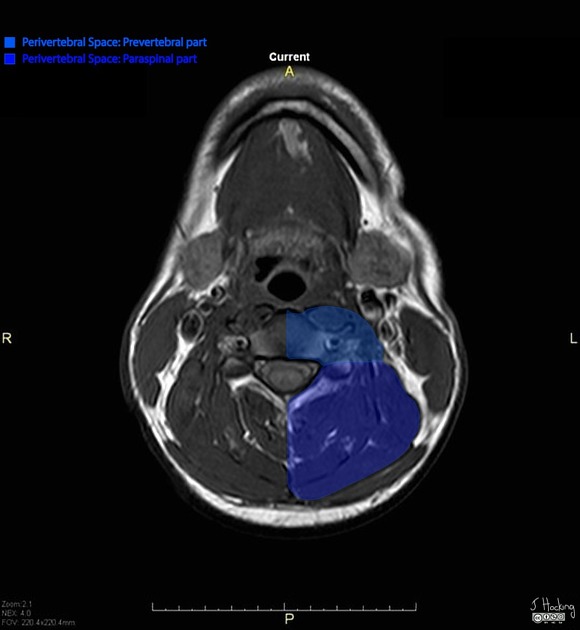
The perivertebral space is one of the deep compartments of the head and neck and includes the prevertebral space and paraspinal space.
On this page:
Gross anatomy
The perivertebral space is a cylinder of soft tissue lying posterior to the retropharyngeal space and danger space surrounded by the prevertebral layer of the deep cervical fascia and extends from the skull base to the upper mediastinum.
The deep cervical fascia sends a deep slip to the transverse process which subdivides the space into:
prevertebral portion: anteriorly located
paraspinal portion: posteriorly located
Contents
-
prevertebral portion 1
cervical vertebral body and disc
-
rectus capitis anterior and lateralis
-
scalene muscles
vertebral artery and vein
roots of brachial plexus
-
paraspinal portion 1
vertebral arches of cervical vertebrae
-
cervical paraspinal muscles
-
rectus capitis posterior major and minor
obliquus capitis superior and inferior
-
extrinsic back muscles
-
superficial layer of intrinsic back muscles
-
intermediate layer of intrinsic back muscles: erector spinae group
longissimus capitis and cervicis
spinalis cervicis and capitis
-
deep layer of intrinsic back muscles: transversospinalis group
-
Boundaries
anterior: danger space and retropharyngeal space
posterior: fascia attaches to spinous process and ligamentum nuchae
lateral: surrounded by posterior cervical space
superior: base of skull
inferior: the perivertebral space is usually defined from the skull base to superior mediastinum but can be extended to the level of the coccyx
Radiographic features
Normal thickness
In general, the prevertebral component is measured on sagittal imaging as the distance between the anterior border of the vertebral body and the air within the pharynx/trachea.
Naturally there is a near-normal distribution of thickness in normal patients depending on body build and expected variation. As such it is not possible to give a definitive cut off that leads to perfect separation of patients with and those without injury. It is merely a question of what sensitivity and specificity you are willing to accept. For example in one study of plain radiographs yielded the following measurements 7:
C2/3: <7 mm
C6/7: <21 mm
Values above these resulted in a true positive rate of 53% and false positive rate of 5% 7.
Similarly normal values for CT vary, but according to one of the larger series in adults values the thickness of the prevertebral soft tissues are 6:
C1: 8.5 mm
C2: 6 mm
C3: 7 mm
C4/C5: variable due to variable height for cricoid/esophagus
C6: 18 mm
C7: 18 mm
Due to the presence of adenoidal tissue superiorly in children, as well as the smaller size values are different, and more variable. One study found the following upper limit of normal values 8:
-
C2
0-2 years of age: 7.6 mm
3-6 years of age: 8.4 mm
7-10 years of age: 6.8 mm
11-15 years of age: 6.8 mm
-
C6
0-2 years of age: 9.0 mm
3-6 years of age: 9.8 mm
7-10 years of age: 12.1 mm
11-15 years of age: 14.5 mm
A mass arising from the prevertebral portion is centered on the vertebral body or prevertebral muscles, which causes anterior displacement of the muscles as opposed to a mass arising from the retropharyngeal space which would cause flattening of the prevertebral muscles posteriorly against the vertebral body 1.
A mass arising from the paraspinal portion displaces the paraspinal musculature and posterior cervical space fat away from the spine. Extension of malignant and benign lesions into the epidural space from the perivertebral space is common 1.
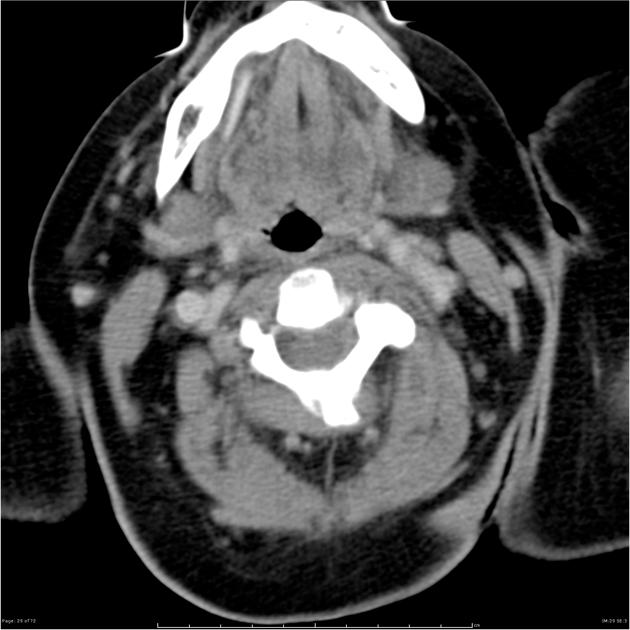
CT
CT is useful to identify details of bone destruction 1
a post-operative or spontaneous abscess can be differentiated from noninfected fluid by signs of rim enhancement as well as fat stranding, muscle swelling and skin thickening around the lesion 3
longus colli tendinitis on CT is characterized by soft tissue swelling in the prevertebral portion anterior to the C2-3 vertebral bodies and associated with calcification in the tendon 1
chordomas are rare and aggressive tumors arising from notochordal remnants in the axial skeleton; on CT the mass is typically hypodense/isodense and associated with lytic vertebral bone destruction and may extend over a number of levels 2
MRI
MRI is the preferred modality for assessing the soft tissue in this space and to detect early infection in the spine 1:
in the acute phase of vertebral osteomyelitis, there is bone marrow edema and this is detected by signal changes with low signal intensity on T1 weighted images (WI) and high signal intensity on T2-WI, especially fat saturated techniques/spectroscopic inversion recovery (SPIR) or short tau inversion recovery (STIR) sequences4
-
lymphoma of the vertebra has been described to have a “wrap-around” sign when tumor was present in the bone marrow and paraspinal soft tissue without alteration in the normal shape of the affected vertebra to help differentiate from lesions of bone metastasis and myeloma which tend to show destruction of the bony cortex and bulging contour
T1: hypointense with high signal post-contrast
T2: hyperintense with contrast enhancement 5
chordomas appear as homogenous hypointense/isointense lesions on T1-WI, hyperintense on T2-WI and show post-gadolinium high signal; tumor develops within the vertebral bodies and frequently invades perivertebral space/epidural space and can span several vertebral segments 2
Related pathology
direct invasion by squamous cell carcinoma
-
pseudotumors
anterior herniated disc







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.