Pulmonary tumour thrombotic microangiopathy occurs when there are non-occlusive tumour cell microemboli with fibrointimal remodelling in small pulmonary arteries, veins and lymphatics. It rarely causes pulmonary hypertension.
On this page:
Epidemiology
Associations
At autopsy, approximately 25% patients with pulmonary tumour thrombotic microangiopathy are found to have an extrathoracic malignancy. Most commonly 6:
- hepatocellular carcinoma
- breast cancer
- renal cell carcinoma
- gastric adenocarcinoma
- prostate carcinoma
- choriocarcinoma
Diagnosis
The diagnosis of pulmonary tumour thrombotic microangiopathy rests upon histological confirmation, most commonly from a lung biopsy 6.
Clinical presentation
Progressive breathlessness is the key symptom of pulmonary tumour thrombotic microangiopathy.
Laboratory tests
- hypoxaemia
- high A-a gradient
- raised D-dimer
Pathology
Thrombotic microangiopathy is a consequence of tumour cells metastasising to the distal tiny arterioles, venules and lymphatics of the lungs. The embolised cells induce an intravascular procoagulant effect resulting in fibrocellular overgrowth of the intima and vasoconstriction. Occasionally, this proceeds to overt pulmonary hypertension.
Radiographic features
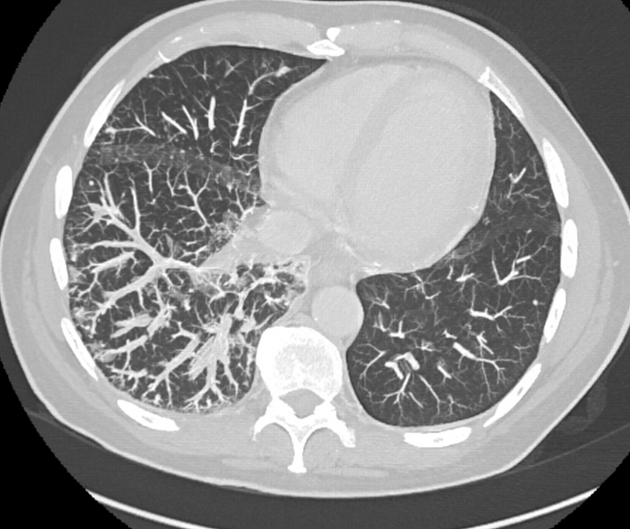
Structural imaging is usually unremarkable in pulmonary tumour thrombotic microangiopathy:
- chest radiography is usually normal
-
CT pulmonary angiography
- unremarkable for pulmonary emboli
- lymphangitis and/or vessel beading may be seen
-
V/Q scintigraphy
- many subsegmental perfusional defects
Treatment and prognosis
Pulmonary tumour thrombotic microangiopathy heralds a dismal prognosis. Although treatment of the primary tumour improves prognosis 6.
History and etymology
It was first described by Von Herbay et al. in 1990 2.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.