Rectus sheath haematomas, as the term implies, occur when a haematoma forms in the rectus abdominis muscle/rectus sheath. It is most common in its lower segment and is generally self-limiting.
On this page:
Epidemiology
Rectus sheath haematomas are more common in women with a 3:1 F:M ratio.
Clinical presentation
Rectus sheath haematomas most often present as acute onset of abdominal pain with a palpable abdominal mass. Additional findings may include fevers, chills, nausea, vomiting, abdominal tenderness, and abdominal guarding. Depending upon the size and location of the haematoma, patients may also present with signs of hypovolaemic shock or even abdominal compartment syndrome 5.
Pathology
Aetiology
The majority of haematomas result from the rupture of epigastric vessels or by tearing of the fibres of the rectus abdominis muscle. This can be due to 1,4:
spontaneously in the context of anticoagulation therapy (most common)
direct or indirect trauma
coagulopathies e.g. cirrhosis
degenerative vascular diseases
iatrogenic, e.g. from high femoral arterial puncture
Radiographic features
Rectus sheath haematomas are classified based upon computed tomography scan findings to guide treatment 6.
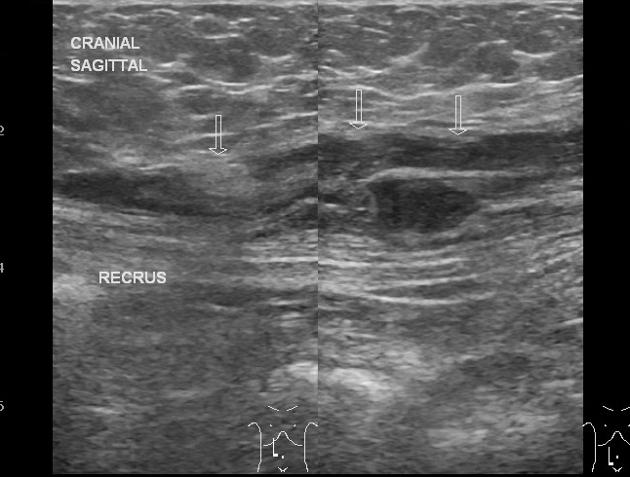
Ultrasound
heterogeneity in rectus abdominis muscle
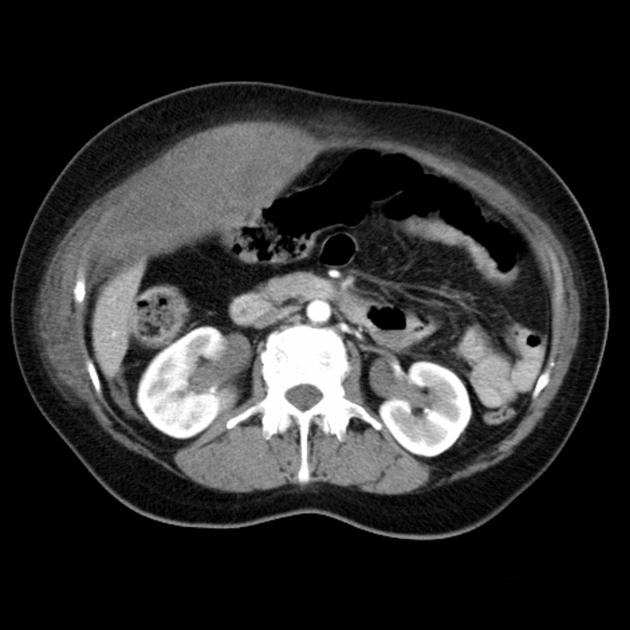
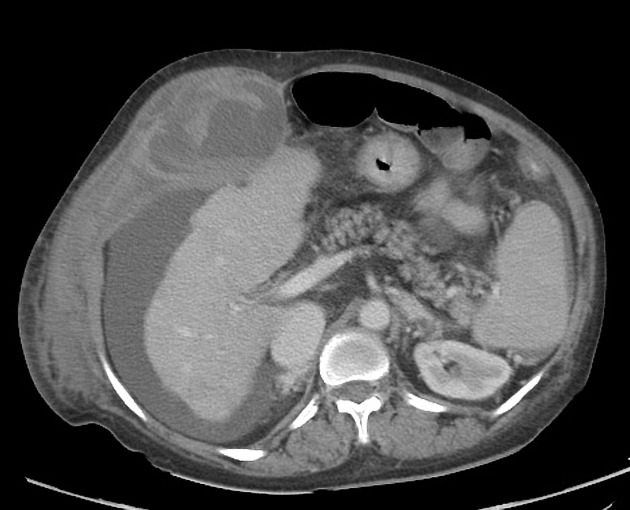
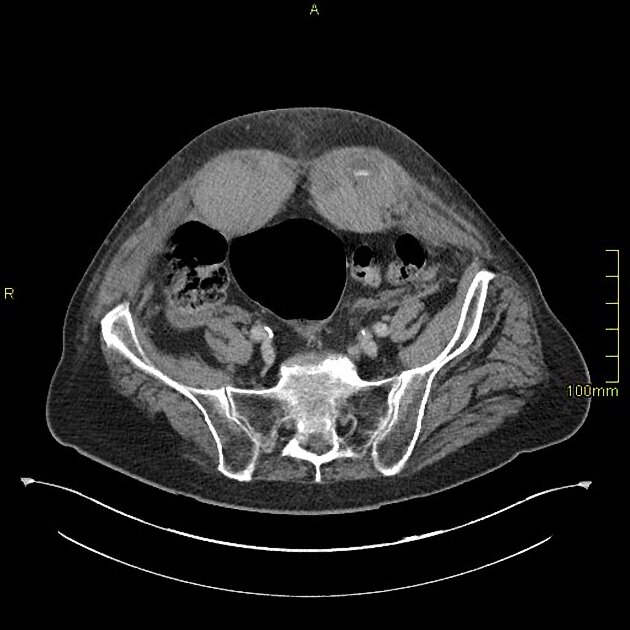
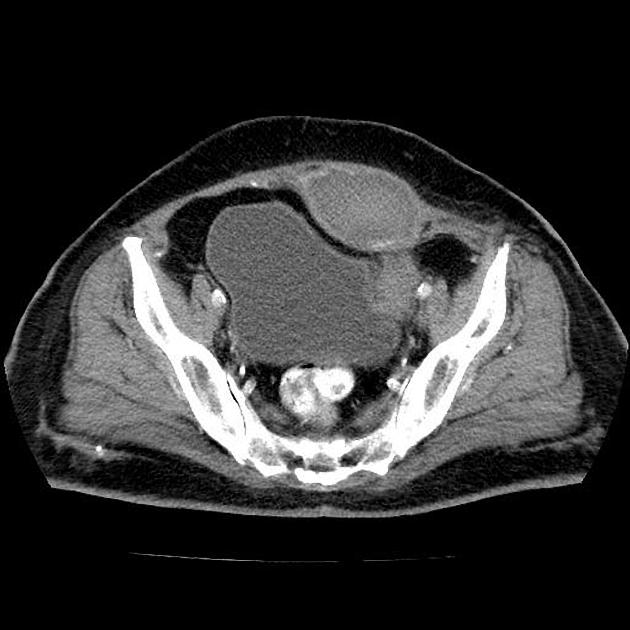
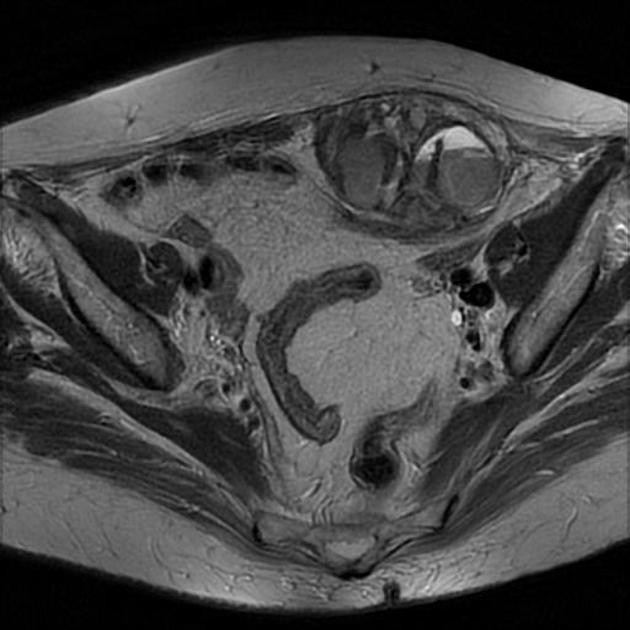
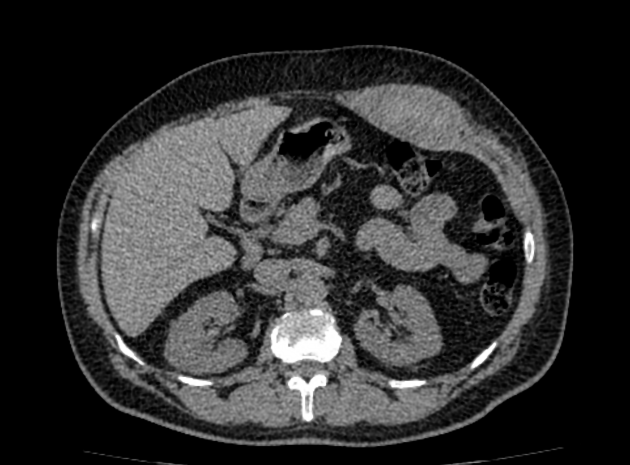
CT
haematoma is confined to the abdominal wall.
high attenuation on unenhanced images
lack of enhancement
resolution on follow-up studies helps confirm the diagnosis
CT classification
type I: small and confined within the rectus muscle; does not cross the midline or dissect fascial planes 6
type II: also confined within the rectus muscle but can dissect along the transversalis fascial plane or cross the midline 6
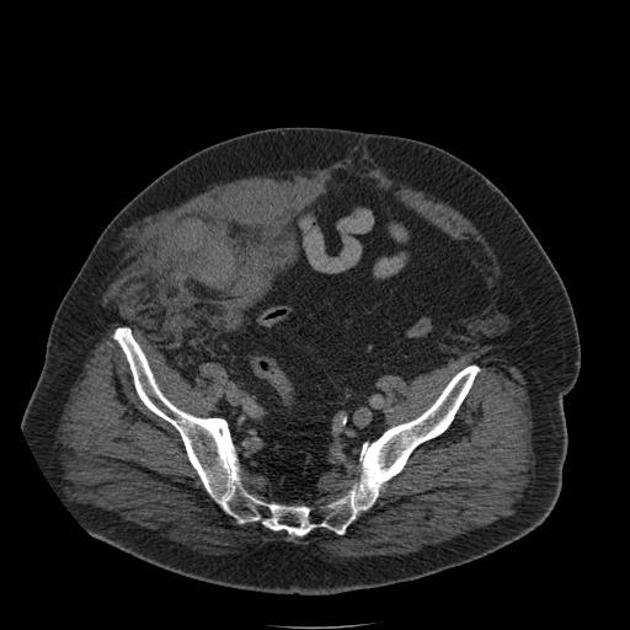
type III: large, usually below the arcuate line, and often presents with evidence of haemoperitoneum and/or blood within the prevesical space of Retzius (retropubic space) 6
Treatment and prognosis
Management of rectus sheath haematoma is determined by the patient's clinical status, the underlying cause, and the classification.
-
type I:
almost all of these patients are haemodynamically-stable without any change in serial haemoglobin or haematocrit levels
patients are treated conservatively with bed rest, analgesia, compression of the haematoma, and reversal of anticoagulation when appropriate 7,8
hospitalisation is not usually required for affected patients
-
types II and III:
patients can present as haemodynamically-stable or show signs of haemodynamic compromise (e.g. altered mental status, hypotension, tachycardia, acute kidney injury, etc.) with an abrupt or gradual decrease in haemoglobin or haematocrit
patients in hypovolaemic shock should be resuscitated aggressively and promptly referred for either angiography with embolisation (first-line intervention at facilities that have interventional radiology capabilities) or surgical ligation of the bleeding source













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.