Renal transplantation (RTx or KTx) is one, if not the most, common transplant procedures undertaken worldwide. Consequently, purposeful and incidental imaging of renal transplants and renal transplant-related complications are increasingly common. These include acute renal transplant rejection and chronic renal transplant rejection. Both donors and recipients undergo a preoperative workup 1.
On this page:
Indications
End-stage renal disease (ESRD) requiring dialysis. Causes include:
most common aetiologies are diabetes and hypertension
-
other causes can be broadly grouped but are not limited to 2:
Pre-renal causes: renal artery stenosis, vasculitis, emboli, renal vein thrombosis
-
Intrinsic renal causes:
Primary glomerular disease: IgA nephropathy, membranous nephropathy, focal segmental glomerulosclerosis (FSGS)
Secondary glomerular disease: autoimmune (e.g. systemic lupus erythematosus), infection (e.g. HIV), drugs, neoplasia
Tubulointerstitial disease: autoimmune (Sjögren's syndrome, tubulointerstitial nephritis and uveitis (TINU)), infection, drugs, sarcoidosis, chronic hypercalcaemia/hyperkalaemia, cystinosis, polycystic kidney disease
Post-renal cause: reflux nephropathy
Types
The two main types of transplants are based on the donor 3:
living donor (usually a relative)
-
deceased donor (more common):
DBD: donation after brain death
DCD: donation after cardiac death
Combined organ transplantation are usually from a deceased donor:
-
double kidney transplant
Ipsilateral or bilateral
combined liver - kidney transplant
heart and kidney transplant
-
pancreas and kidney transplant
Kidney and islet transplant: islets are injected into the portal system and engraft into the liver parenchyma
Radiographic features
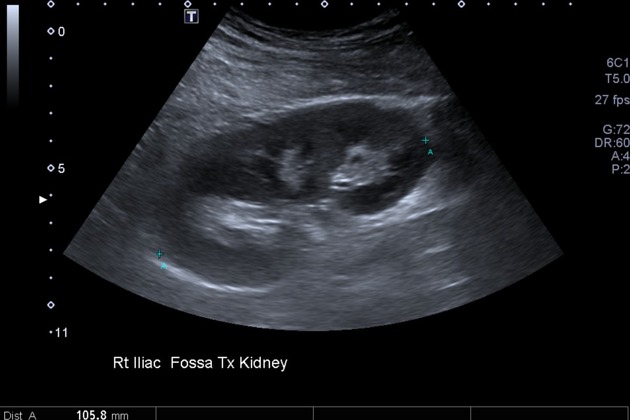
Most renal transplants are sited in the extraperitoneal tissues of the right iliac fossa and usually anastomosed to the external iliac vein and either iliac artery. For a variety of surgical reasons (including vessel suitability or previous failed renal transplants), they may occur in the left iliac fossa or elsewhere.
Plain radiograph
renal transplant not often visualised directly as obscured by other soft tissues of the pelvis but may be visible if calcified (i.e. failed)
surgical paraphernalia such as clips and ureteric stents may be visible
complications related to underlying disease, or the renal transplant and its associated anti-rejection medications (e.g. osteonecrosis)
Ultrasound
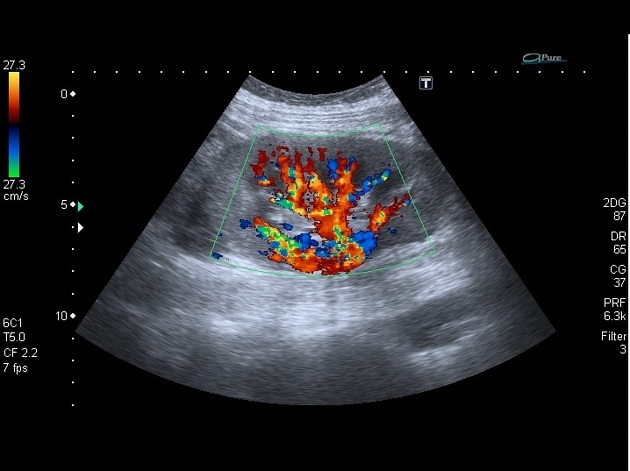
Renal transplant ultrasound is commonly utilised to evaluate for complications postoperatively. Read the separate article on this for US features 4.
Magnetic resonance imaging
MRI alongside non contrast enhanced MR angiography is sometimes used, complementary to ultrasound, for better characterisation of complications and delineation of the anastomoses 5.
Renal transplant scintigraphy
Transplant renal scintigraphy is mostly used for the evaluation of urological and vascular complications (renal transplant complications), and postoperative fluid collections (renal transplant fluid collections) 6.
Practical points
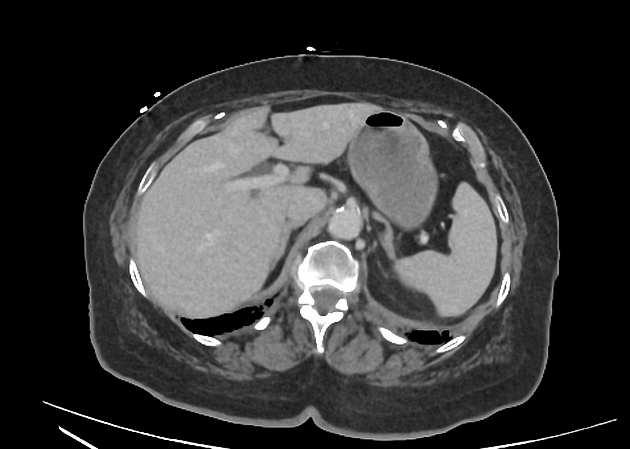
The preoperative workup should include a chest and abdominal x-ray, an abdominal ultrasound, an echocardiogram and coronary stress tests. However, in most patients, an abdominal CT is also useful to evaluate arterial calcifications and calibre (especially of the right external iliac artery) 7. Spectral ultrasound may be used to define the haemodynamics of vessels. For those with a history of thrombosis (e.g. a DVT), doppler ultrasound may be required to exclude ongoing clot burden 5.













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.