Seminal vesicle cyst
Updates to Article Attributes
Seminal vesicle cysts can be congenital or acquired.
Congenital
Epidemiology
ItAge of presentation of congenital cysts is during the presenceperiod of greatest reproductive activity i.e in second and third decades of life, while acquired cysts withinare most often seen in the seminal vesicles since birth
Clinical presentation
Smaller cysts may be detected incidentally. It is seen rarely and occurs probably due to an obstruction atIn symptomatic patients, the junction of the seminal vesicle and ejaculatory duct. It is associated with many other urogenital anomalies:
-
renal agenesisor dysgenesis1 -
ectopic insertion of ureter into seminal vesicleusual presenting features include perineal pain,ductus deferensabdominal pain, ejaculatoryduct or prostatic urethra ductus deferens agenesis
Acquired
This occurs secondary to the obstructionpain, dysuria, haematuria, increased frequency of the seminal vesicle causing cystic dilatation.
-
obstruction bybenign prostatic hypertrophy -
chronic infectionmicturition, urinary tract infections andscarring of the seminal vesicle or ejaculatory duct prior prostate surgery-
autosomal dominant polycystic kidney disease5
Pathology
Aetiology
Congenital
Congenital cysts occur due to insufficient drainage as a result of atresia of the ejaculatory ducts causing distension of seminal vesicles and further leading to the formation of a cyst. They usually become symptomatic in young adulthood due to the accumulation of secretions. These cysts are mostly unilateral with no predilection for the side of involvement
Congenital cysts are associated with many other urogenital anomalies:
- renal agenesis or dysgenesis 1
- ectopic insertion of ureter into seminal vesicle, ductus deferens, ejaculatory duct or prostatic urethra
- ductus deferens agenesis
- Zinner syndrome
Acquired
Acquired cysts are seen most often secondary to prostatic infection or surgery causing scarring and finally obstruction of the drainage of secretions. This is seen most often bilaterally.
Associations
- obstruction by benign prostatic hypertrophy
Clinical presentation
Age
Radiographic features
Seminal vesicles appear normal or enlarged in size with presence of cysts within.
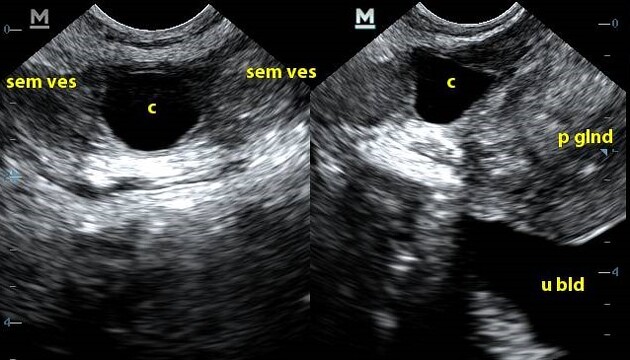
Ultrasound
These can be imaged by transabdominal ultrasound and are best evaluated by transrectal ultrasound. The cysts may be anechoic or may contain internal debris from haemorrhage or infection.
CT
Larger cysts may be seen on CT. The cysts may be seen as well defined, low attenuation lesions or thickthick and irregular walled cysts with hyperdense contents in cases of secondary haemorrhage or infection. These lesions are classically located in the retro-vesicular region and cephalic to prostate. The associated renal anomalies can be depicted well.
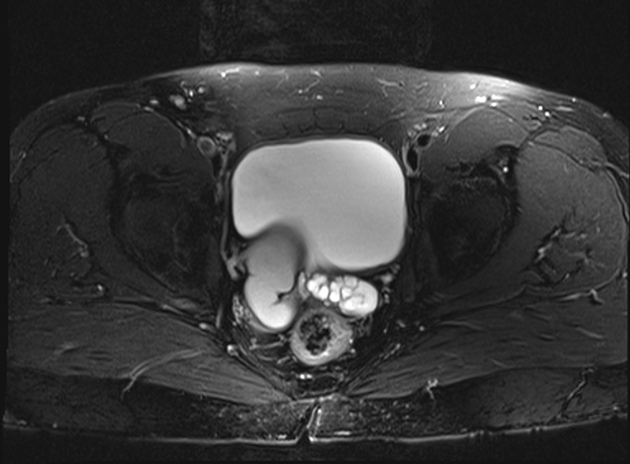
MRI
Best in differentiating cystic pelvic lesions. Abdominal and pelvic anatomy can also be assessed. Classical appearance of cysts is maintained with low T1 and high T2 weighted signal intensity. Some seminal vesicle cysts may have high T1 and T2 signals probably due to proteinaceous contents or haemorrhage.
Treatment and prognosis
Depending on the size of the seminal vesicle cyst, surgery may be done.
Differential diagnosis
Other causes of male pelvic cystic masses can be included as a differential diagnosis.
-
MullerianMüllerian duct cyst - seen in the midline - ejaculatory duct cyst - seen in the midline
- prostatic cysts
- diverticulosis of ampulla of vas deferens - lateral in location
- ectopic ureterocele
References changed:
- 5. Danaci M, Akpolat T, Baştemir M et al. The prevalence of seminal vesicle cysts in autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 1998;13(11):2825-8. <a href="https://doi.org/10.1093/ndt/13.11.2825">doi:10.1093/ndt/13.11.2825</a>
- 5. Wolfgang Dähnert. Radiology Review Manual. (2011) <a href="https://books.google.co.uk/books?vid=ISBN9781609139438">ISBN: 9781609139438</a><span class="ref_v4"></span>







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.