Seminal vesiculitis is an uncommon entity characterised by inflammation of the seminal vesicles. It is most commonly infective in aetiology and often associated with concurrent infection elsewhere in the male genital tract, forming part of the spectrum of male accessory gland inflammation 4. It is usually acute, although a chronic form is well-recognised 7.
On this page:
Epidemiology
There is a lack of good data on the incidence and prevalence of seminal vesiculitis. However, one small study demonstrated that it was found in almost 25% of patients with synchronous urethritis 1.
Risk factors
absent/decreased secretion of semenogelin I 5,6
Clinical presentation
The spectrum of symptomatology of seminal vesiculitis is broad:
-
ejaculatory dysfunction
painful ejaculation (odynorgasmia)
seminal hyperviscosity
decreased ejaculate volume
-
pain
pelvic
flank
abdominal
groin
abdominal swelling
Physical examination of the seminal vesicles is difficult due to their location, and even on digital rectal examination (DRE), with a long index finger, it can be technically-challenging to palpate the glands, especially if the bladder is distended.
Laboratory analysis:
-
urinalysis
haematuria
pneumaturia
infection (e.g. leucocytes, nitrites, etc.)
-
seminal fluid analysis may show
oligospermia/azoospermia
seminal hyperviscosity
decreased ejaculate volume
Pathology
The pathogenesis of seminal vesiculitis remains confused, with an unclear relationship between it and other infective conditions of the male excurrent ductal system, e.g. chronic prostatitis, urethritis, acute epididymitis.
Thus organisms that cause/contribute to these infective entities are also thought to play a role in vesiculitis, e.g. Chlamydia trachomatis
In relevant endemic regions, tuberculosis and schistosomiasis may both produce a chronic form of vesiculitis 9.
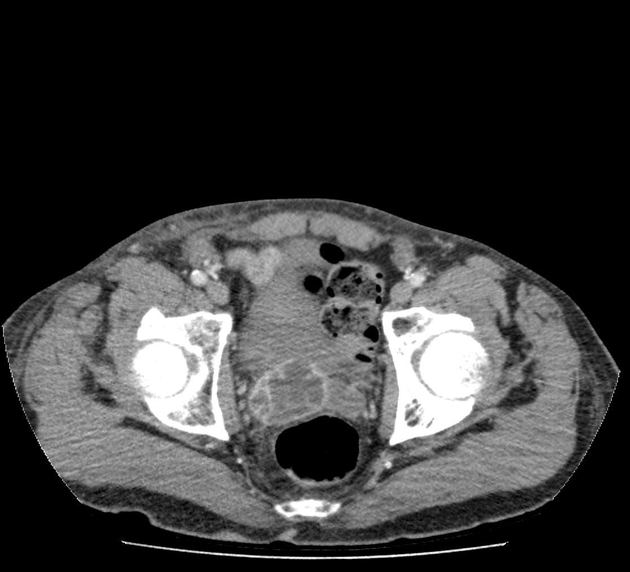
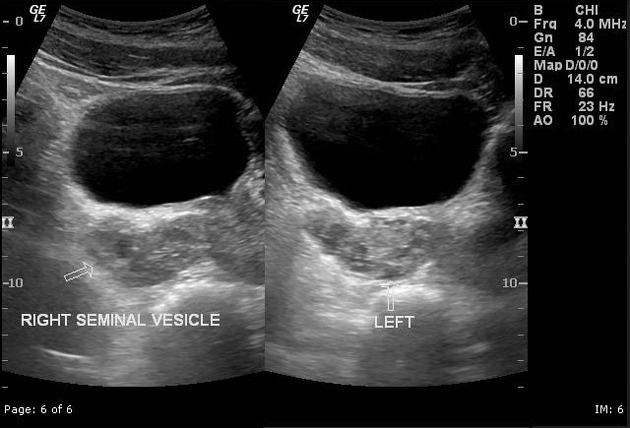
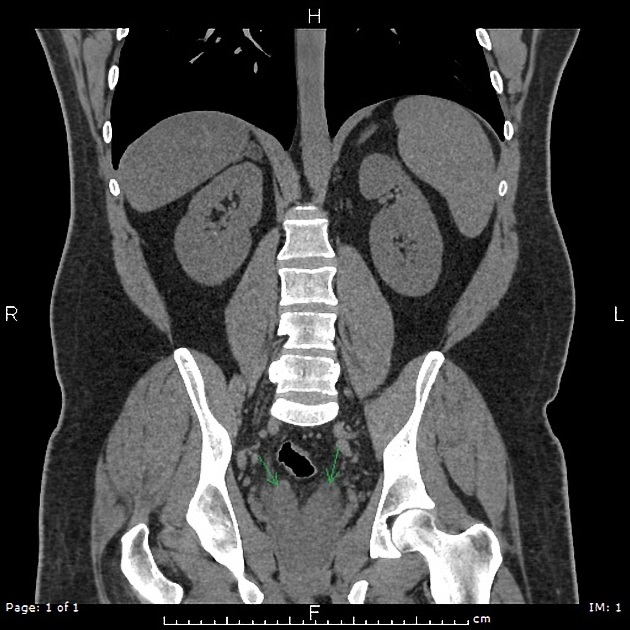
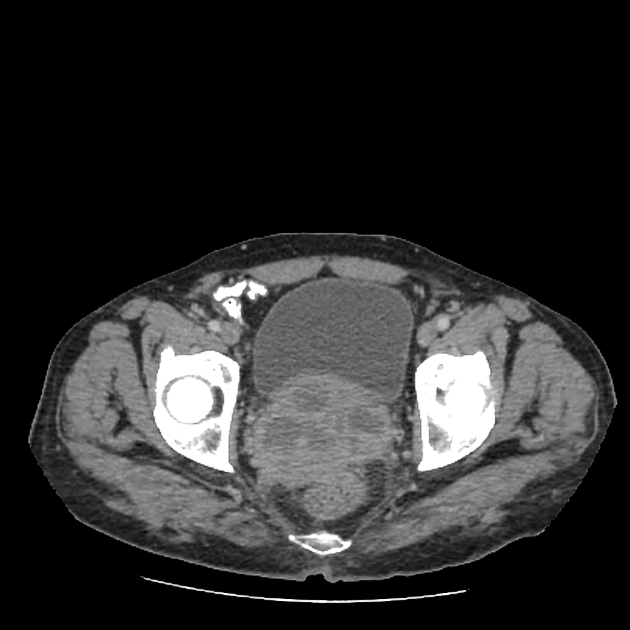
Radiographic features
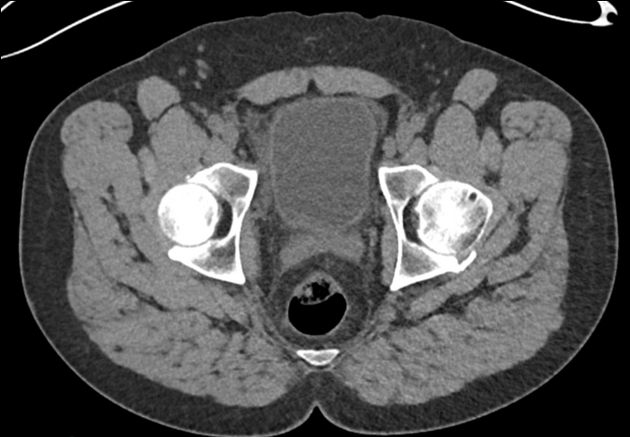
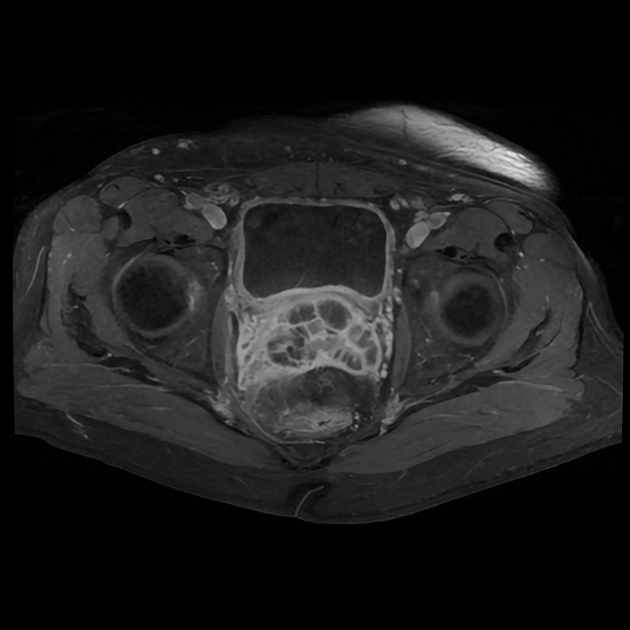
TRUS/CT/MRI
diffuse mural thickening of the seminal vesicles
acute disease: dilatation of the seminal vesicular tubules
chronic disease: atrophy of the seminal vesicular tubules
-
CT/MRI
diffuse enhancement of the walls or septa
Treatment and prognosis
Acute seminal vesiculitis may respond to antibiotics. Chronic vesiculitis can be much more tricky to treat.
There is a risk of untreated/undertreated seminal vesiculitis progressing to a seminal vesicle abscess.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.