This is a basic article for medical students and other non-radiologists
Skull fractures usually occur following significant head injury and may herald underlying neurological pathology.
On this page:
Reference article
This is a summary article; read more in our article on skull fractures.
Summary
-
anatomy
-
epidemiology
accurate incidence and prevalence unknown
-
1.3 million traumatic brain injuries per year in the USA 1
estimated that 1/3 will have a skull fracture
-
presentation
head injury following impact trauma, e.g. fall, RTC
-
symptoms associated with underlying injury
-
there may be an associated base of skull injury
Battle sign (bruising over mastoid process)
raccoon eyes
-
pathophysiology
-
mechanism
children and elderly: simple fall
adults: usually high-energy impact trauma, e.g. RTC
-
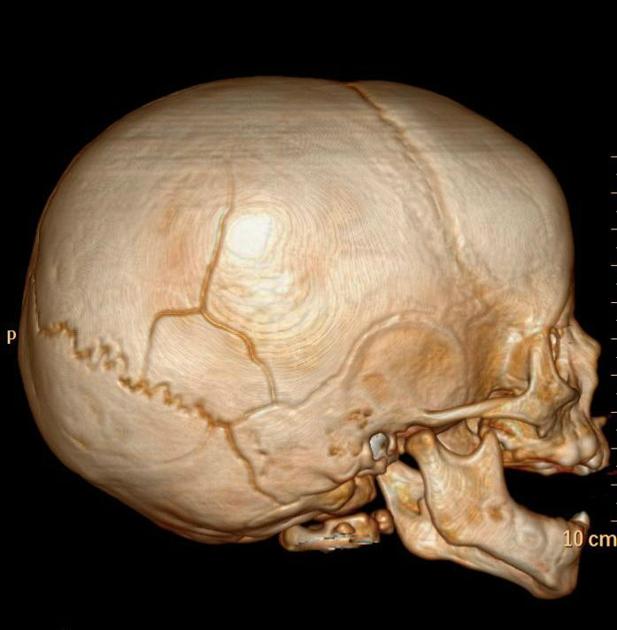
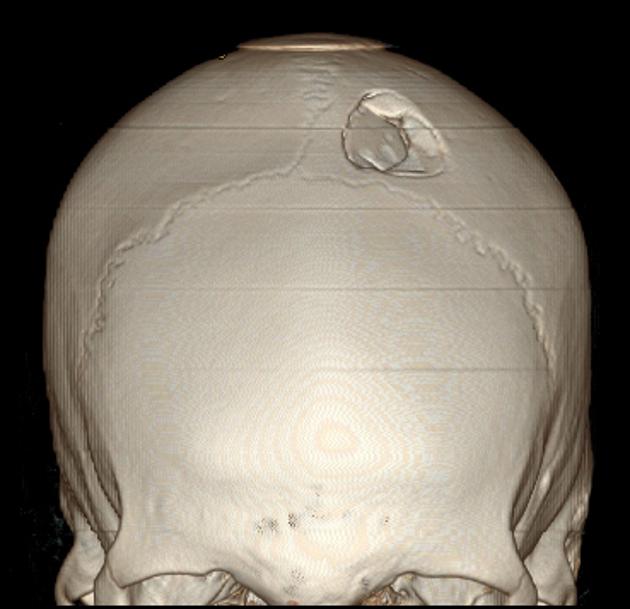
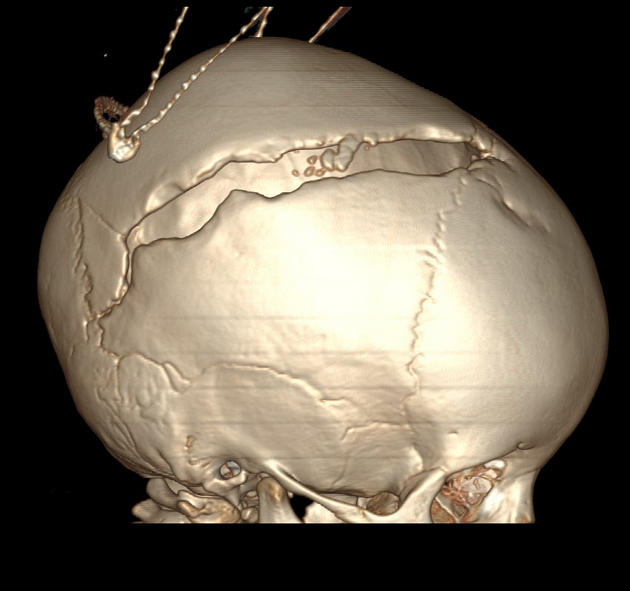
different types of fractures
linear
base of skull fracture
diastatic (widening suture lines in childhood)
-
associations
bone fragments under the fracture
other penetrating injuries
-
-
treatment
-
head injury patients should be treated following ATLS (or similar)
C-spine control and ABCDE
assessment of Glasgow coma scale (GCS)
-
treatment depends on the type of fracture
linear: no specific treatment
depressed: may require neurosurgical intervention to prevent further brain injury
base of skull fracture: may be unstable and require expert
-
Imaging
-
role of imaging
-
diagnosis of fracture
skull x-rays are still performed but are being used less and less
CT head is the first line investigation
-
assessment for intracranial injury, e.g. hemorrhage
-
assessment of the need for imaging using a clinical scoring system
NICE guidance
-
assessment of fracture to guide risk stratification and management
-
-
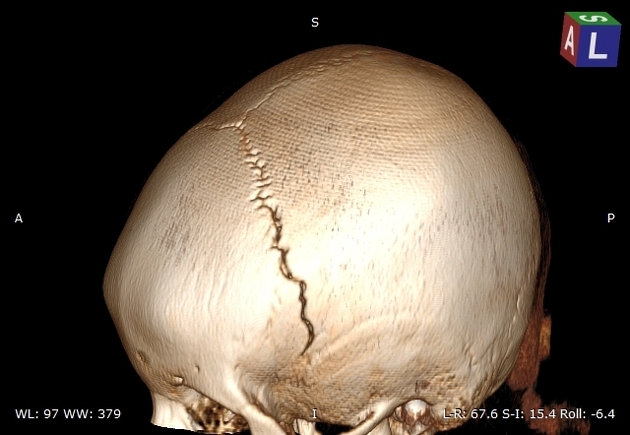
radiographic features
-
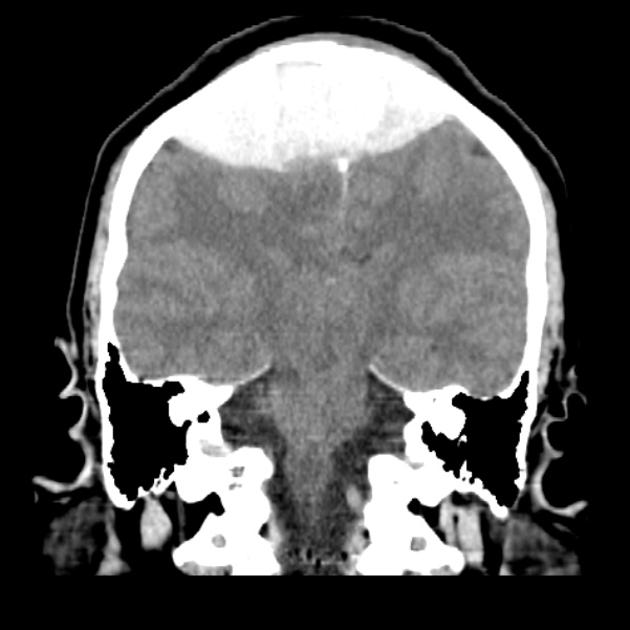
CT
best method for looking for bony injury
best test for looking at extra-axial collection or brain injury
allows assessment for other signs, e.g. pneumocephalus
review on different windows (brain, blood, bone)
3D reconstruction
-






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.