Spinal epidural haematomas are rare and can result in severe morbidity if treatment is delayed and they are thus typically considered a surgical emergency.
On this page:
Clinical presentation
The patient's symptoms and signs will depend on the location of the haematoma, and the degree of spinal cord/cauda equina compression. Typically there will be a combination of severe pain and neurological deficit. See spinal cord injury and cauda equina syndrome for more information.
Pathology
Spinal epidural haematomas are most commonly spontaneous venous bleeds, often in the setting of coagulopathy or over-anticoagulation. They are anatomically located in the space between the theca and the periosteum - known as the extradural neural axis compartment.
Aetiology
-
spontaneous: most common 4
especially in the context of a bleeding disorder or over-anticoagulation
trauma, e.g. vertebral fracture
iatrogenic, e.g. lumbar puncture, epidural anaesthesia
spinal arteriovenous malformations or other vascular anomalies
pregnancy
Location
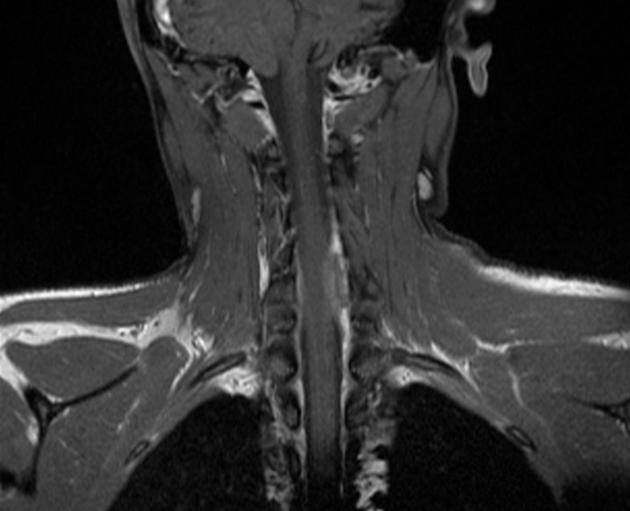
Spinal epidural haematomas can occur throughout the spine but are most common in the cervicothoracic region, usually posterior to the thecal sac over 2-4 vertebral levels 1,4.
Radiographic features
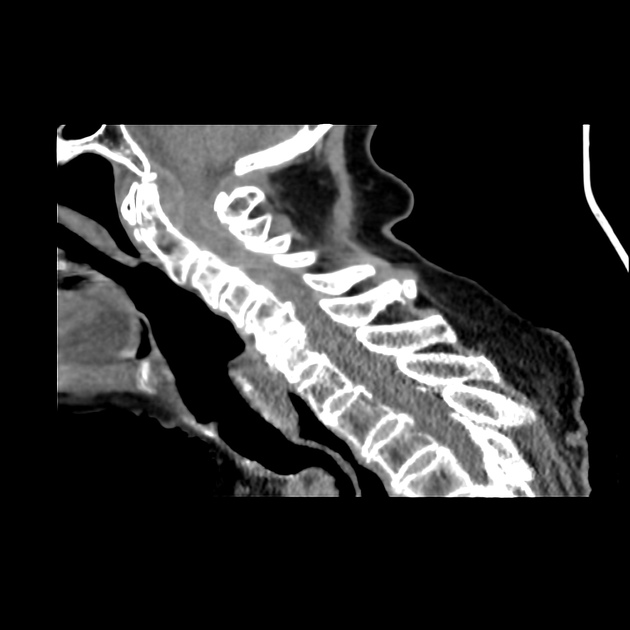
CT
non-contrast: hyperdense (50-70 HU) extradural mass 4
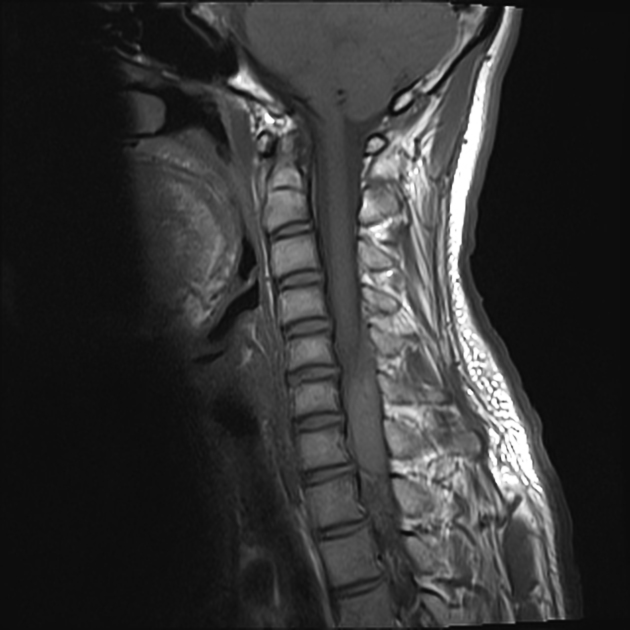
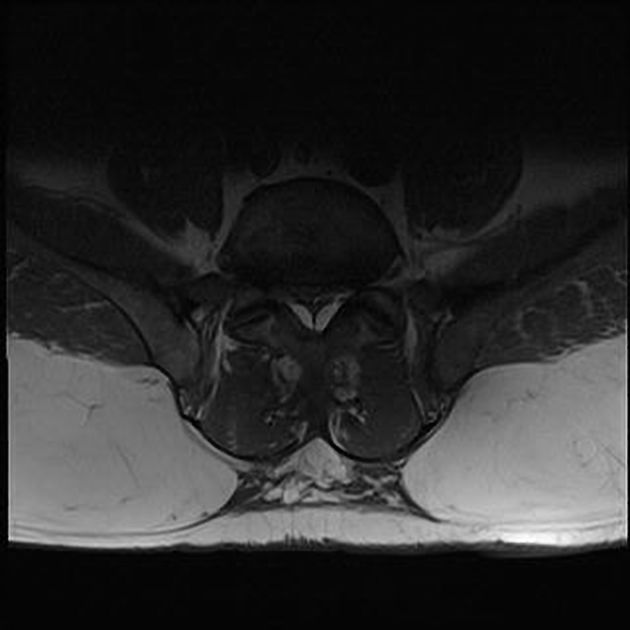
MRI
Signal characteristics will vary on the age of the blood. Signal characteristics of acute spinal epidural haematomas 1,2,5:
T1: isointense or hyperintense to spinal cord
T2: heterogeneously hyperintense to spinal cord with hypointense foci
SWI/T2*: blooming artifact
Differential diagnosis
Practical points
assessment of spinal cord compression and spinal nerve roots should always be done.










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.