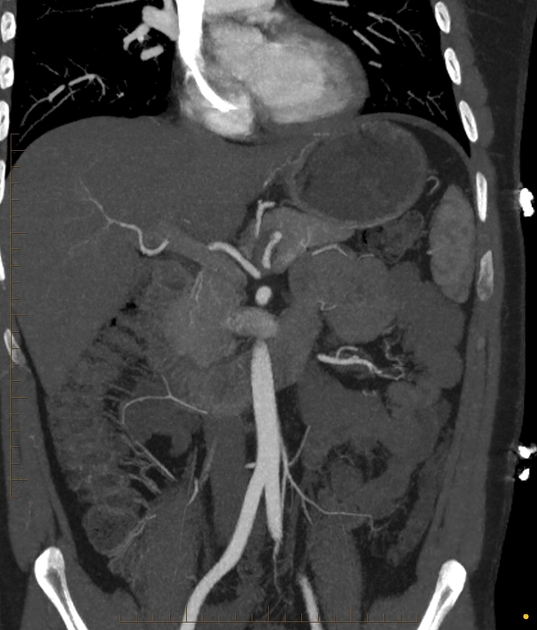
Splenic artery pseudoaneurysms are rare and can arise from any portion of the splenic artery and its branches.
On this page:
Clinical presentation
Unlike splenic artery true aneurysms, splenic artery pseudoaneurysms will nearly always present with symptoms 2. While their occurrence may be higher, fewer than 200 cases of splenic artery pseudoaneurysms are reported in the English literature (c. 2007) 2.
Pathology
While they are sometimes grouped under splenic arterial aneurysms, they are distinct entities and different from the splenic artery true aneurysms. In contrast to a true aneurysm, the pseudoaneurysm wall contains only the intimal and medial layers 2.
Their size can vary; if >5 cm, they are called giant splenic artery pseudoaneurysms 3.
Etiology
They usually occur as a complication of 1,2:
pancreatitis: pancreatic enzymes are thought to cause a necrotizing arteritis with destruction of vessel wall architecture and fragmentation of elastic tissues
trauma: pseudoaneurysms are more often intraparenchymal and rarely involve the main splenic artery
iatrogenic and postoperative causes
peptic ulcer disease (rare)
Radiographic features
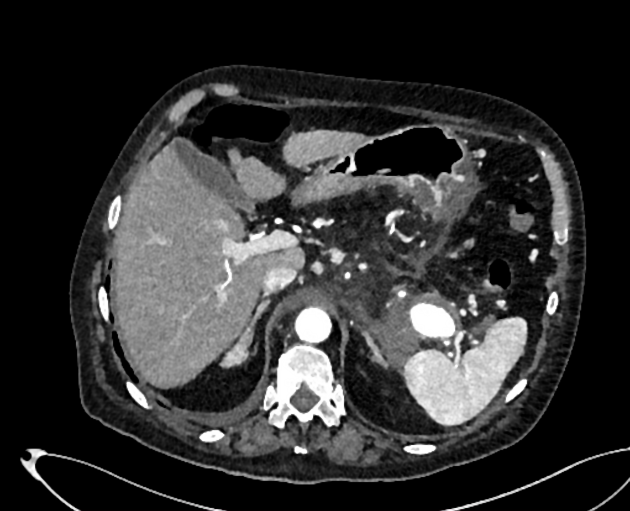
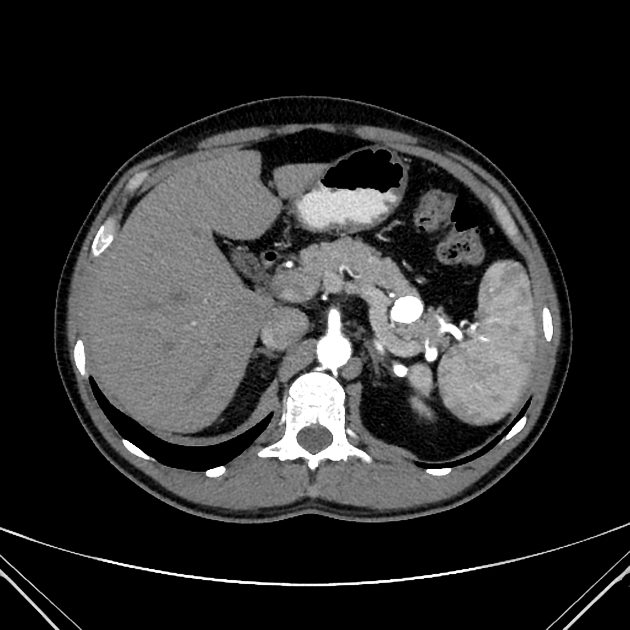
CT
CT is the modality of choice in assessing splenic trauma:
true aneurysms will appear just as they do at other locations
intraparenchymal pseudoaneurysms have a similar appearance to active hemorrhage on initial scanning but do not increase in size on delayed phases and follow the blood pool on all phases
intraparenchymal pseudoaneurysms and AV fistulas have a similar appearance and cannot be differentiated on CT
in contrast, active hemorrhage appears as a high density (80-95 HU) material due to the extravasation of IV contrast media that increases in size on delayed imaging
Treatment and prognosis
Compared to true splenic artery aneurysms, splenic artery pseduoaneurysms grow a relatively more rapid rate and have a higher potential for rupture 5. Surgical or endovascular treatment of splenic artery aneurysms is recommended regardless of size 5.






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.