The term synostosis (plural: synostoses) refers to the fusion of bones usually at cartilaginous or fibro-osseous connections. Synostoses occur physiologically, as asymptomatic anatomical variants or might be abnormal and cause clinical symptoms as a functional loss. The latter is clinically significant and might need treatment.
Physiological synostoses occur as a result of ossification of synchondroses or syndesmoses with advancing age and include the following:
physeal closure of primary and secondary ossification centers
synostoses of the sacral vertebra
synostoses of pubic, ischial and iliac bones (acetabulum, ischiopubic)
synostoses of the sternal body segments
synostosis of the mandibular synchondrosis
Synostoses can exist as anatomical variants that are rarely associated with symptoms and include the following:
lumbosacral transitional vertebra (Castellvi type III and IV)
Abnormal synostoses can be congenital or acquired, can occur as complications following trauma or surgery, or intended postsurgical outcomes. They include the following clinical conditions 1-5:
humeroradial synostosis
osseous carpal coalition or tarsal coalition
spondylocarpotarsal synostosis syndrome
complete joint ankyloses
On this page:
Epidemiology
Epidemiological data depend on the location or type of the synostosis and on whether they are congenital or acquired and seem to vary significantly between different populations.
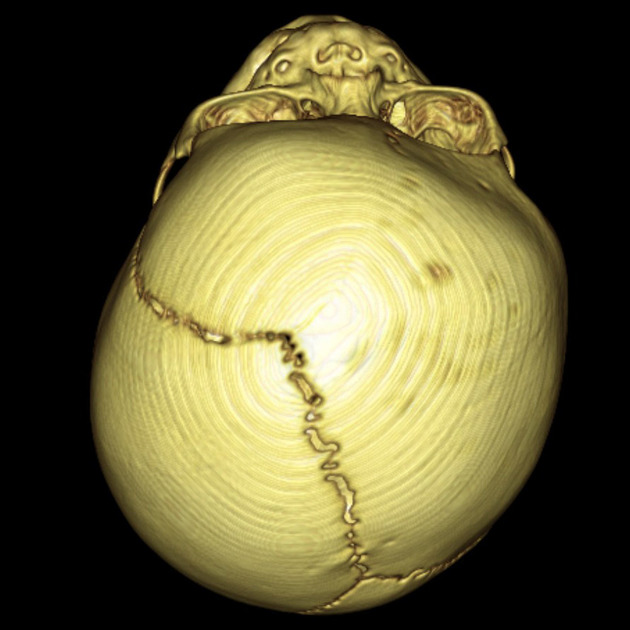
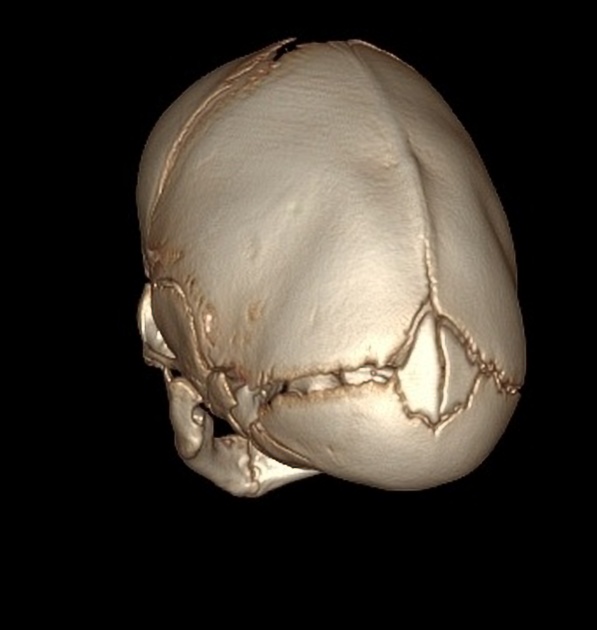
The reported incidence of congenital cervical vertebral synostoses varies between 0.5 and 6.25% 4, the frequency of occipitocervical synostoses is less common ranging between 0.08% and 3% 5. Craniosynostosis has a reported incidence of 0.4-05% 6,7. Both congenital radioulnar and tibiofibular synostosis are rare conditions 8-11. Carpal and tarsal coalitions are again more common with an estimated frequency of 0.1% to 8% depending on the population in carpal coalitions 12 and about 1% of tarsal coalitions 13,14, where synostoses make up about one-third of talocalcaneal coalitions 14.
Acquired synostoses can occur as rare complications of forearm or ankle fractures. Posttraumatic radioulnar synostosis has been reported in up to 2% 2 and distal tibiofibular synostosis in up to 5% after transsyndesmotic or suprasyndesmotic ankle fractures (AO type 44-B or 44-C) 15.
Associations
Synostoses might be associated with the following conditions 2,3:
-
cranial trauma
surgery
infection (osteomyelitis, septic arthritis, tuberculosis)
Risk factors
Predisposing factors for acquired synostoses include trauma and treatment-related factors such as 2,3:
-
fractures of two adjacent bones
comminuted fractures and/or fractures at the same level
open fractures with significant soft tissue injury
bone fragments on the interosseous membrane
associated cranial trauma
prolonged trauma-to-surgery interval
prolonged immobilization
delayed rehabilitation
Diagnosis
The diagnosis of synostosis can be easily confirmed with imaging such as plain radiographs or CT.
Clinical presentation
Also depending on the type and location synostoses might be asymptomatic or can present with deformity and functional loss or decreased range of motion 2,3. Incomplete synostosis can present with pain 2.
Pathology
Etiology
Synostoses can be congenital or acquired. Some of the congenital synostoses have been linked to genetic disorders 4.
Location
Synostoses tend to occur at cartilaginous or fibro-osseous connections between two adjacent bones.
Subtypes
Synostoses can be classified based on their location.
Radiographic features
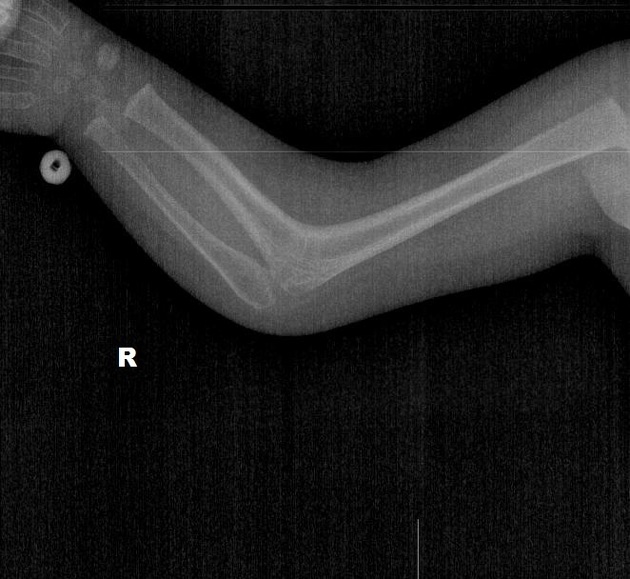
Plain radiograph
Plain radiographs can easily confirm and depict the synostosis as an osseous fusion between adjacent bones.
Ultrasound
Ultrasound might show a cortical bridge but is unable to assess the deep located bony structures.
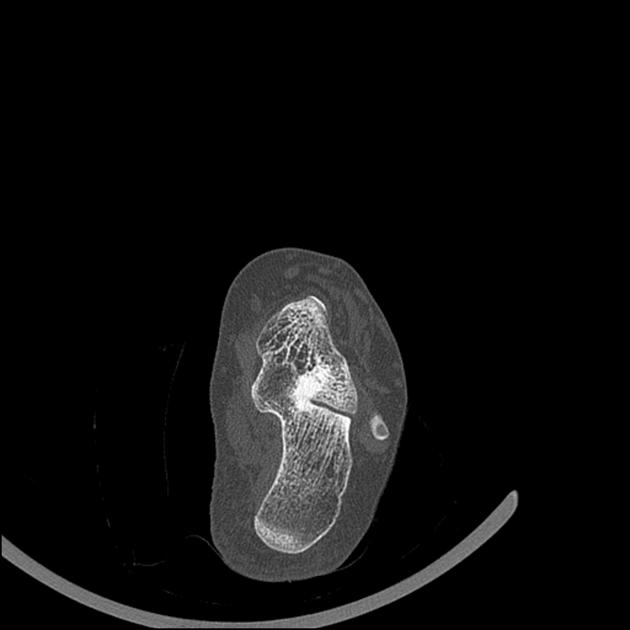
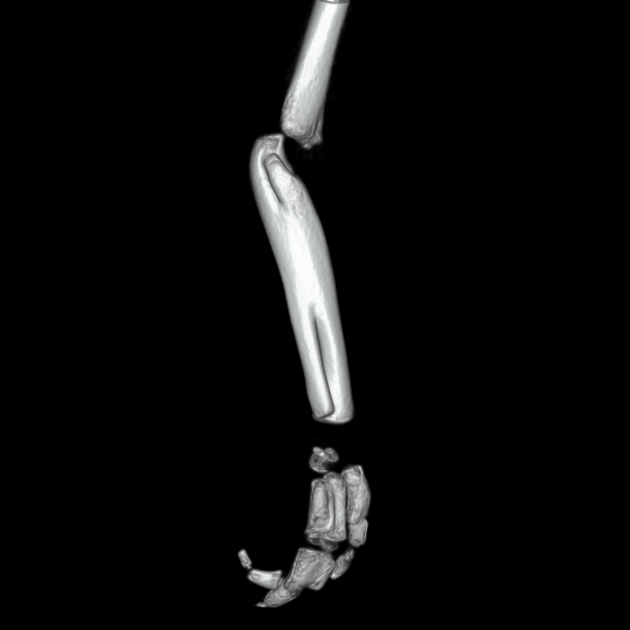
CT
CT can precisely demonstrate the location and extent of the synostosis by complete fusion of trabecular and cortical bones.
MRI
Complete synostosis is demonstrated by osseous fusion and a continuous bridge of the cortical and cancellous bone as well as the bone marrow signal. In addition, MRI can depict bone marrow edema or soft tissue edema indicating incomplete synostosis.
Nuclear medicine
A bone scan can show the maturation and activity of the synostosis.
Radiology report
The radiological report should include the description of the following:
an osseous bridge between two adjacent bones
associated bone marrow edema
associated soft tissue edema or soft tissue abnormalities
Treatment and prognosis
Management and prognosis of synostoses will depend on the location, type and extent and associated clinical symptoms 2,3. Any physiological synostoses and asymptomatic variants will not require treatment whereas craniosynostosis or posttraumatic radioulnar synostosis might require surgery 2. The development of distal tibiofibular synostosis after ankle surgery on the other hand has been shown to not significantly alter the surgical outcome and therefore will probably also not require further treatment 3.
History and etymology
Spinal vertebral fusions have been already described by Greek historians 15. The first tarsal coalition has been described by Georges-Louis Leclerc, Comte de Buffon in 1769 13. The first proximal radioulnar synostosis was reported by the Dutch anatomist Eduard Sandifort in 1793 8,9. Craniosynostosis were first precisely categorized by Rudolph Virchow in 1851 16 and the first talonavicular synostosis was reported by RJ Anderson in 1879 17.











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.