Vanishing white matter disease (VWM), also known as childhood ataxia with central hypomyelination (CACH), is a rare, genetic leukoencephalopathy due to EIF2B subunit mutations, typically appearing as extensive white matter involvement with cavitary changes.
On this page:
Epidemiology
Most cases are encountered in young patients with onset in early childhood or adolescence being typical 1. A number of adult patients have, however, been described 4.
Presentation is preceded by minor head trauma or infection resulting in episodic deterioration followed by incomplete and slow recovery 1. With repeated episodes, patients accumulate neurological impairment eventually succumbing to the disease 1.
Clinical presentation
The diagnosis is made on the basis of clinical and MRI appearances, as no established diagnostic laboratory tests exist 1.
Diagnostic criteria have been proposed 3:
psychomotor development is normal or near normal initially
onset of neurologic deterioration is episodic with chronic progressive course, and occurs in childhood
-
neurologic signs typically include:
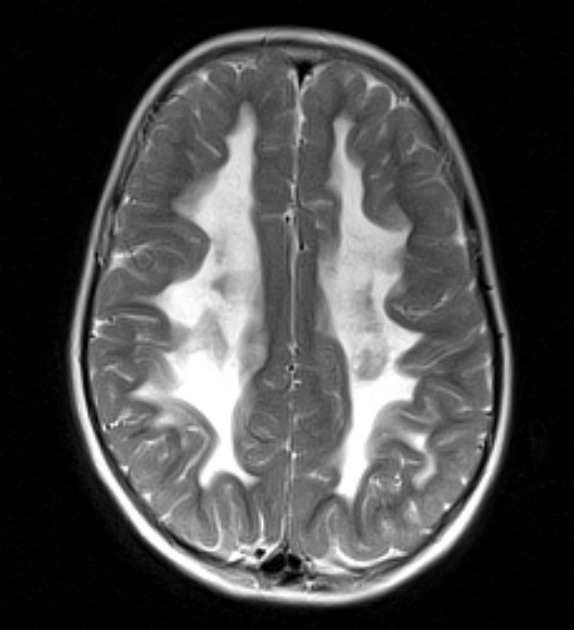
imaging (MRI) bilateral and symmetric cerebral hemispheric white matter signal intensity similar to CSF
For the diagnosis to be made, all four criteria should be identified 3.
Pathology
Vanishing white matter disease is a leukodystrophy characterised by astrocytic dysfunction 5.
Microscopic appearance
Histology reveals the following 1:
rarefaction of the white matter (more severe in the deeper white matter)
microcystic change in the periventricular white matter
spongiform change in the arcuate fibres and the corpus callosum
neuronal loss is not present
Genetics
Vanishing white matter disease is caused by mutations in any of the genes EIF2B1, EIF2B2, EIF2B3, EIF2B4, or EIF2B5 (most common) that encode the five subunits of the eukaryotic translation initiation factor 2B (eIF2B); each have a different chromosomal locus 5.
Radiographic features
MRI
MRI is the modality of choice for assessing cases of possible vanishing white matter disease and other white matter diseases.
White matter is diffusely involved with T2/FLAIR hyperintensity, extending from periventricular white matter to the subcortical arcuate fibres. Over time, the white matter vanishes replaced by near-CSF intensity fluid (i.e. it attenuates on FLAIR) 1.
Cerebellar atrophy is variably present and ranges from severe to mild and typically involves the vermis 3.
MR spectroscopy is useful. In affected white matter, only lactate and glucose peaks remain. In unaffected grey matter, the trace is near-normal with small glucose and lactate peaks 1.
Treatment and prognosis
Although the disease is spontaneously remitting, each episode results in accumulation of further injury. No treatment has been identified and death usually occurs within months to years (range: few months to 14 years) 1.
Differential diagnosis
When a potential case is encountered, it is unusual for the reading radiologist to have had any significant personal experience with the disease, and as such a differential needs to be entertained, including 3:
-
leukodystrophies, especially: Alexander's disease
deterioration is not episodic
patients are usually macrocephalic
white matter is affected in a fronto-occipital gradient
histology: Rosenthal fibres are present







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.