Patient Data
Note: This case has been tagged as "legacy" as it no longer meets image preparation and/or other case publication guidelines.

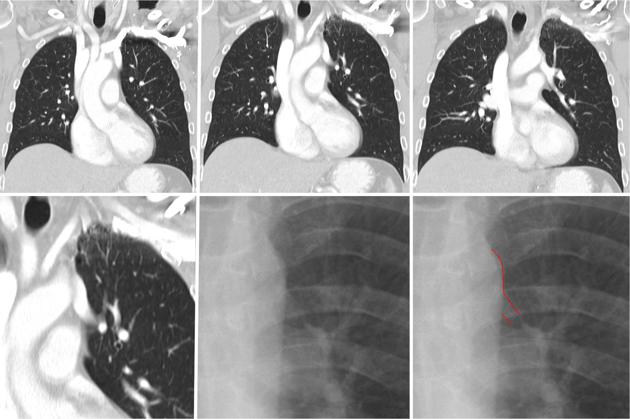
Prominent left mediastinal border vascular shadow.


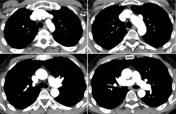

The left upper pulmonary vein is draining into the left brachiocephalic vein.
Case Discussion
Partial anomalous pulmonary venous return (PAPVR) has a prevalence of 0.5% in the general population1. Anomalous pulmonary vein drains into the pulmonary circulation via the superior vena cava (SVC), azygos, innominate veins, inferior vena cava (IVC), coronary sinus or right atrium) creating a pulmonary-to-systemic shunt 1,2.
Patients may be asymptomatic if the shunt is small. However, when the shunt is large or when there is associated cardiopulmonary anomalies, the patient may be symptomatic 1,2. The most common configuration is when the right upper lobe pulmonary vein drains into SVC or - as in this case - a left upper lobe pulmonary vein draining into left innominate vein 1. Surgical correction is suggested if the pulmonary-to-systemic flow ratio is greater than 1.5 to avoid late sequelae of pulmonary hypertension and right ventricular failure 1,2.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.