Presentation
5 days progressive lower limb weakness, now in acute urinary retention. Known poorly controlled SLE.
Patient Data


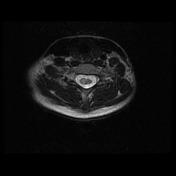



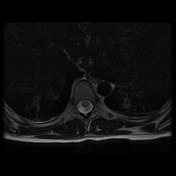






Extensive areas of T2 high signal throughout the cervical and thoracic cord predominantly involve the central grey matter, although in sections extend to areas of white matter. None of these regions demonstrate contrast enhancement, however, faint leptomeningeal enhancement is demonstrated along the entire superficial surface of the cord including the posterior fossa structures.
In the context of SLE, longitudinally extensive cord signal abnormality with smooth mild leptomeningeal enhancement most likely represents SLE related transverse myelitis or NMO spectrum disorder. Viral/post viral transverse myelitis is also a differential.
Laboratory investigations:
- ESR 97 (2-12)
- double stranded DNA antibodies 358 IU/mL (0-4)
- C3/C4 low
- EBV/CMV/HBV/mycoplasma/HIV serology - no evidence infection
- NMO serology - negative
Case Discussion
The current understanding of myelitis in individuals with systemic lupus erythematosus (SLE) includes a distinction between two clinical pictures and pathogenetic mechanisms for the development of myelitis.
- SLE myelitis: a rapid onset severe neurological deficit occurring in the context of clinical and laboratory evidence of active SLE. This has poor prognosis and is thought to have a thrombotic/ischemic etiology.
- Co-existent neuromyelitis optica (NMO): more subacute onset of neurological deficit which is responsive to immunosuppressive therapy but has a relapsing course, often associated with optic neuritis. Markers of SLE activity such as ESR are often within the normal range, and NMO antibody is present. Up to 50% of patients with NMO have a co-existent autoimmune condition, most commonly SLE or Sjogren's syndrome.
In this case, the elevated ESR with C3 and C4 depletion are consistent with active SLE, while absence of NMO antibody makes NMO unlikely.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.