Presentation
Recurrent upper abdominal pain
Patient Data




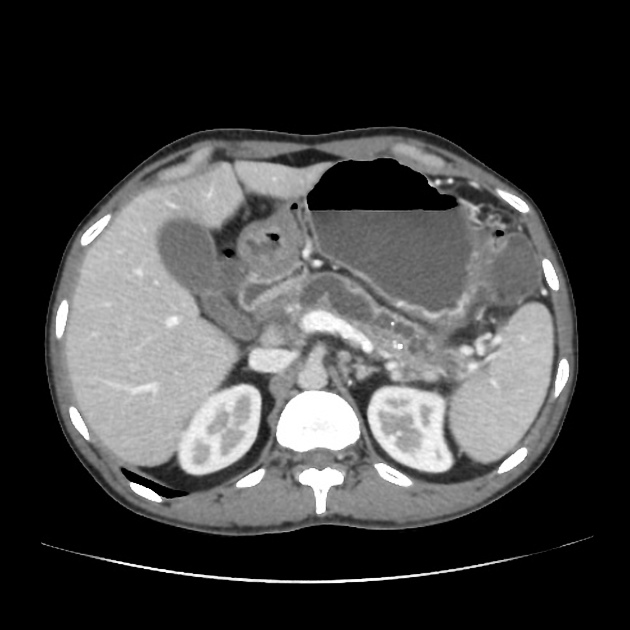
Generalized atrophy of body and tail of the pancreas. Diffuse parenchymal calcification with main pancreatic duct dilated throughout its course with a beaded appearance reaching up to 10mm in diameter. Multiple intraductal calculi are present, the largest measuring 10 mm in the pancreatic head. This stone is obstructing the main pancreatic duct resulting in ductal dilatation. No hypoenhancing pancreatic parenchymal lesions. No peripancreatic fat stranding or localized collections. No radio-opaque stones in the gallbladder, cystic duct, or common bile duct. No intrahepatic biliary duct dilatation.
Case Discussion
When presenting with an episode of abdominal pain, this patient underwent an ultrasound of the abdomen which revealed features of chronic calcific pancreatitis. However, due to the suboptimal acoustic window, a CT scan was recommended to rule out any pancreatic inflammation or neoplasm. The chronic inflammatory changes result in reduction in volume of pancreatic parenchyma with only a ghost of the gland remaining in the latter stages. These patients are more prone for neoplasms and have to be watched closely.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.