Presentation
Status reanimation due to thrombotic occlusion of the LAD and subsequent coronary stent one month prior. Known bilateral serial rib fractures. Now presents again with atypical chest pain and epigastric pain. ECG with T-wave negativity in several leads, but unchanged compared to her post-infarction ECG.
Patient Data










Technique
patient premedication: beta blocker and nitrates
acquisition method: step and shoot (prospective acquisition)
contrast injection protocol: triphasic injection
standard image reconstruction
Findings
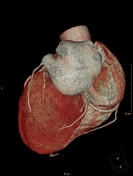
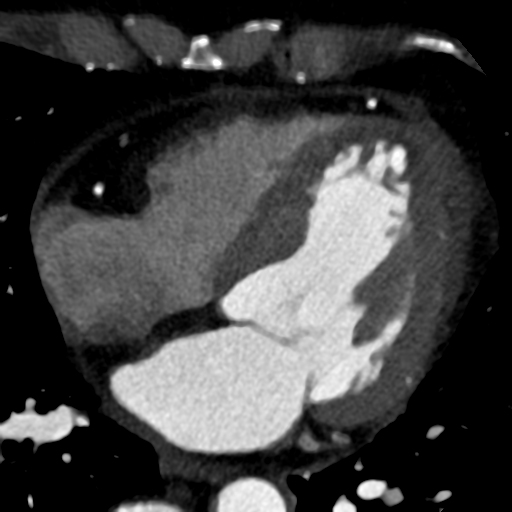
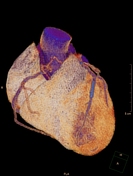
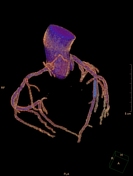
normal coronary origins and proximal courses
right coronary dominance
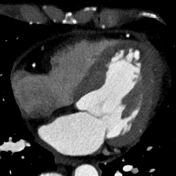
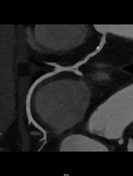
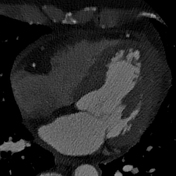
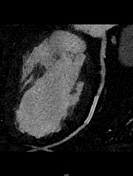
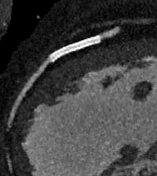
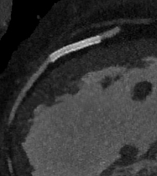
coronary stent in the distal LAD
Plaque burden:
calcium score (according to Agatson, not shown): 33
segment involvement score (SIS): 2 segments
Right coronary artery (RCA): duplication from mid-segment
small eccentric calcified plaque with slight wall irregularities and mild stenosis in the proximal segment
strong posterolateral branch
Left main (LM): small eccentric plaque, quadrifurcation
Left anterior descending artery (LAD): strong D1 and small rudimentary D2
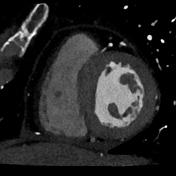
coronary stent in the distal segment - estimated stent lumen 1.5-2 mm
regular opacification in front and behind the stent
Ramus intermedius (IM): two branches - a tiny and large branch that supply the basal lateral wall
Circumflex artery (CX): inconspicuous
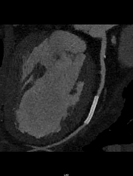
Other cardiac findings:
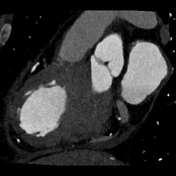
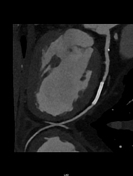
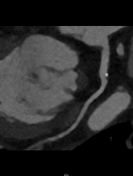
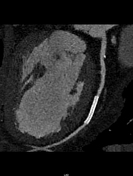
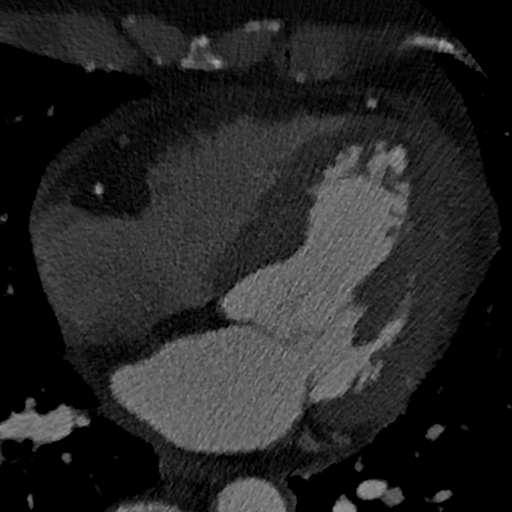
small subendocardial perfusion defects at rest in the anterior wall apically
small pericardial effusion most prominent around the left lateral free wall
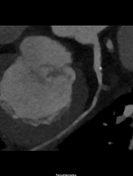
underwashed intracardiac thrombus (~2 x 1cm) of the left ventricular apex
Impression
mild single-vessel coronary artery disease
coronary artery stent in the distal LAD - no stent occlusion/thrombosis
mild pericardial effusion
intracardiac thrombus in the left ventricular apex
Exam courtesy: Yvonne Kühn (imaging technologist)












Technique
sharp reconstruction algorithm
curved and straight multi-planar reconstruction
-
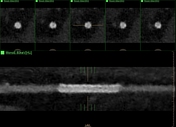
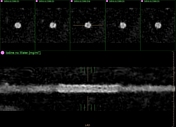
dual-energy reconstructions:
conventional - window setting C800 W2000
monoE 80 keV - window setting C800 W2000
iodine no water - window setting C20 W40
Findings
The stent lumen with a lumen diameter of ~2.0 mm measured on PACS on the oblique images (bone window) outer diameter ~2.75 mm.
The assessment concerning in-stent stenosis is still slightly difficult due to the small stent lumen, but probably feasible. There is surely no evidence of stent occlusion, though.
Case Discussion
This case demonstrates options for visualizing the lumen of a coronary stent in a patient with a history of thrombotic occlusion of the distal left anterior descending artery and subsequent coronary intervention, who now came back with chest pain.
Coronary stent: drug-eluting stent, size 2.75 mm according to the manufacturer.
After interdisciplinary discussion, a careful review of all image reconstructions and all current clinical parameters (including the absence of elevated high-sensitive troponins), it was decided that this is good enough to rule out significant in-stent stenosis.
The pericardial effusion decreased slightly during the hospital course.
Because of the secondary incidental finding of an intracardiac thrombus, she was immediately put on anticoagulation.
A gastroscopy was performed due to clinical suspicion of a stress ulcer, which revealed a hiatus hernia and antral gastritis. The atypical pain was attributed to the gastritis as well as the known serial rib fractures for which the patient was receiving appropriate therapy including pain management.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.