Presentation
Umbilical discharge and lower abdominal pain. Past history of cholecystectomy and recent history of laparoscopic umbilical hernia repair.
Patient Data

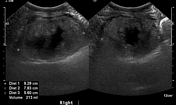



There is a well-defined mass in the right flank that appears echogenic with a central hypoechoic area.
At the umbilicus, surgical threads/sutures are seen in association with a turbid ill-defined fluid collection and related areas of increased vascularity on color flow.


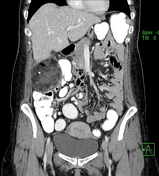




There is a well-defined heterogenous low attenuation mass containing fat density demonstrating capsular enhancement. It is located anteromedial to the lower pole of the right hepatic lobe, anterior to the right kidney and lateral to the hepatic flexure of the colon. Within the mass, a linear hyperdense foreign body is seen with an appearance similar to the surgical clips in the gallbladder bed.
At the umbilicus, there is a fluid collection containing a few gas foci denoting postoperative abscess formation.
Case Discussion
Encapsulated omental infarction (necrosis) is an unusual benign inflammatory process that can be secondary to abdominal surgeries, trauma or pancreatitis. The differential diagnosis for encapsulated omental fatty lesions may also include peritoneal liposarcoma and foreign body granuloma. Encapsulated omental infarction can become infected and may develop into an abscess 1-4.
This patient had a history of cholecystectomy a few years earlier and a recent history of laparoscopic umbilical hernia repair, after which she complained of umbilical discharge and vague lower abdominal pain.
Ultrasound examination of the abdomen revealed postoperative umbilical inflammatory collection and right lumbar heterogenous mass, for which a contrast-enhanced CT was recommended.
CT revealed an encapsulated fatty lesion inseparable from the right colon. The patient underwent surgical excision of the mass and the right colon. Pathological results revealed a mass of fat necrosis and abscess formation as well as colonic intramural inflamed sinuses and foreign-body granuloma.
Umbilical hernias in adults are usually secondary to increased intra-abdominal pressure as in pregnancy, obesity, ascites and intra-abdominal masses 5. In this patient, the umbilical hernia may have developed secondary to the mass that could be a sequel of the earlier cholecystectomy.
Case courtesy: Prof. Dr. Yasser Ragab




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.