Presentation
Diffuse abdominal pain and diarrhoea, with no fever or associated vomiting. As an important clinical record, the patient had chronic ischaemia of inferior extremities treated with aortobifemoral bypass.
Patient Data
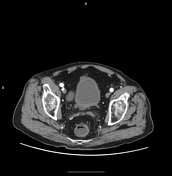

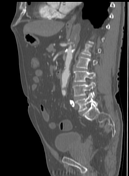


An urgent CT scan showed thrombosis of the proximal segment of the superior mesenteric artery.

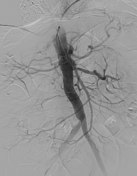
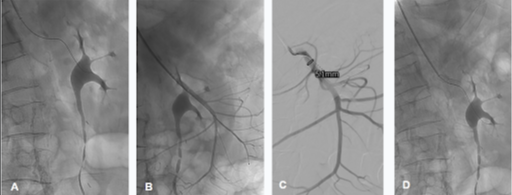
An aortogram, performed through the left axillary access with 6Fr introducer, showed opacification of the coeliac trunk and repletion defect of the proximal segment of superior mesenteric artery (fig. 2a). Selective catheterisation of superior mesenteric artery followed by arteriography confirmed proximal stenosis associated with thrombosis (fig. 2b) and 50.000 IU of urokinase was administered. The following arteriography showed disappearance of the image suggestive of thrombosis. However, the image suggestive of proximal stenosis persisted (fig. 2c).
Therefore, it was decided to place two overlapping stents to cover the length of stenosis. Given that there was no superior mesenteric artery opacification visualised in arteriography (fig. 2d), it was decided to perform intravascular ultrasound (OptiCross 60MHz coronary imaging catheter 3.0F (1.00 mm) x 135 cm) where the permeability of superior mesenteric artery and the stents could be verified (see ultrasound images).
The realisation of the ultimate arteriography confirmed the permeability of prosthesis with adequate stent deployment.

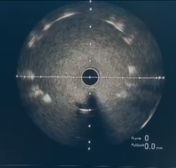
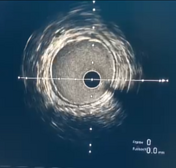

Intravascular ultrasound imaging (OptiCross 60MHz Coronary Imaging Catheter 3.0F (1.00 mm) x 135 cm) where the permeability of superior mesenteric artery and the stents were verified:
intravascular ultrasound catheter positioned in the descending aorta
intravascular ultrasound catheter positioned in the proximal segment of SMA where the prosthesis-associated artifact is visualised
intravascular ultrasound catheter positioned in the post-stent segment of SMA
Case Discussion
Conventional arteriography provides information in a single plane of the vascular lumen and has limited capacity to accurately and reproducibly measure vessel stenosis and characterise plaque morphology.
Intravascular ultrasound, on the contrary, offers cross-sectional images of the arterial lumen and wall, providing a more detailed analysis of vessel structure and greater sensitivity in detecting diffuse and concentric atherosclerosis as a cause of superior mesenteric artery stenosis. Similarly, some studies have also demonstrated the higher sensitivity of intravascular ultrasound in detecting arterial dissection as a complication of angioplasty.
Thus, in our clinical case, where evaluation by conventional arteriography proved to be limited, intravascular ultrasound was crucial in guiding the subsequent clinical and therapeutic decisions during the procedure.
This case is submitted in collaboration with Dr. Landa, Dr. Codina, and Dr. Preciado.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.