Presentation
Incidental left adrenal mass.
Patient Data






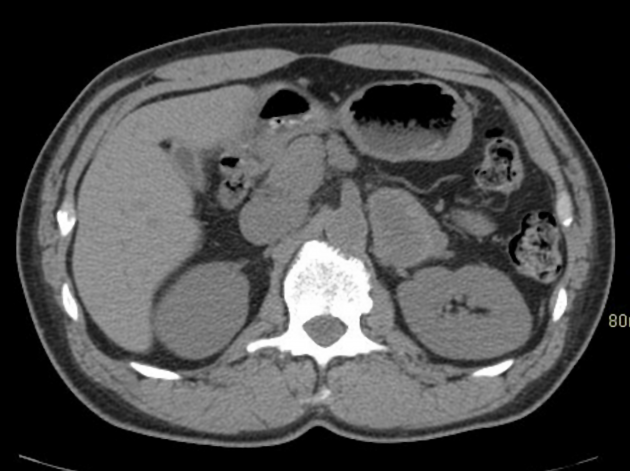
Pre and post-contrast CT performed for haematuria shows a 4.9 cm mass in the left adrenal gland. The mass is centrally cystic or necrotic and demonstrates enhancement of the soft tissue rim.
The lesion was concerning for adrenal cortical carcinoma or metastasis of unknown primary.







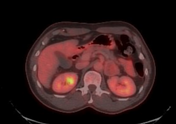


F-18 FDG PET-CT shows the left adrenal mass has only mild FDG avidity, less than the liver. No extra-adrenal primary or other suspicious findings are present.
Findings are not supportive of adrenal cortical carcinoma or metastasis and an I-123 MIBG scan was recommended to assess for possible phaeochromocytoma.






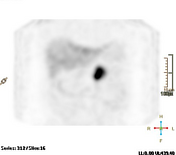


A whole-body I-123 MIBG scan with SPECT-CT was obtained 24 hours after radiotracer administration.
I-123 MIBG scan shows intense radiotracer uptake by the left adrenal mass. No other non-physiologic sites of radiotracer uptake are present.
Findings are most consistent with a phaeochromocytoma.
Final diagnosis post left adrenalectomy: phaeochromocytoma..
Case Discussion
I-123 MIBG is a sensitive imaging modality for the detection of phaeochromocytoma, estimated 79-96%, with higher rates seen in benign and non-metastatic diseases.
18F-FDG has lower sensitivity for detection of phaeochromocytoma but may outperform MIBG in the setting of malignant metastases.
As in this case, phaeochromocytoma imaging by these two radiotracers may be discordant with MIBG-positive FDG-negative lesions being better differentiated whereas MIBG-negative FDG-positive lesions are more dedifferentiated.
MIBG is taken up by relatively benign functioning phaeochromocytoma; malignant disease has less functional tissue and a higher metabolic rate.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.