Presentation
Hemoptysis.
Patient Data






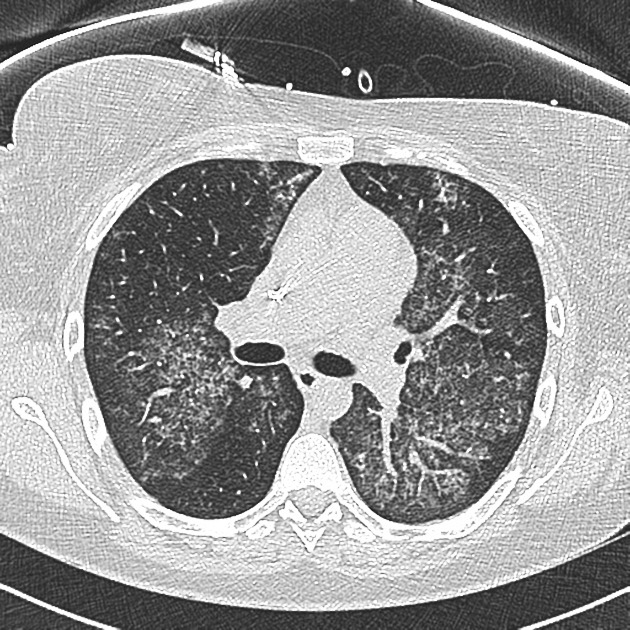
There are confluent ground-glass densities within both lungs, predominantly in a central distribution, with sparing of the subpleural lung.
No septal thickening demonstrated. No pleural effusion or lymphadenopathy. Right-sided central venous catheter noted in situ. No bony abnormality demonstrated.
Conclusion
There is bilateral ground-glass infiltrate. The main differential for this includes pulmonary hemorrhage and atypical infection. Pulmonary edema is less likely, although non-cardiogenic edema could also be considered.
Case Discussion
The patient is known to have perinuclear pattern of antineutrophil cytoplasmic antibodies (p-ANCA) vasculitis. Bronchoscopy revealed extensive blood on both sides. No organisms isolated.
Pulmonary hemorrhage is very uncommon in polyarteritis nodosa (PAN), the lungs are usually spared. Hemorrhage is more often seen in other vasculitides, such as Wegener's or systemic lupus erythematosus (SLE).
In this patient on immunosuppression, the other important differential diagnosis is an opportunistic infection. Bronchoscopy is diagnostic, revealing blood and bronchial washings showing no organisms.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.