Progressive multifocal leukoencephalopathy immune reconstitution inflammatory syndrome (PML-IRIS)
Presentation
New HIV diagnosis, presenting with pneumocystic pneumonia. CD4 count of 0. Eccentric behavior and irritability reported in collateral history. Any evidence of opportunistic intracranial infection?
Patient Data
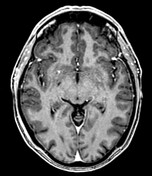
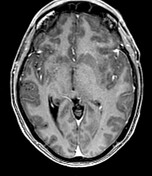
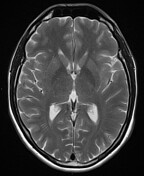
Presentation MRI with CD4 0
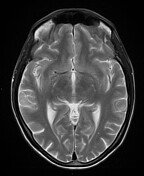





Other than a few tiny deep frontal white matter T2W hyperintensities - which are more than anticipated for age but nonspecific (possible early small vessel changes - intracranial imaging is normal.
No acute abnormalities, with no abnormal diffusion restriction or enhancement.
As part of the HIV treatment, the patient was started on combination antiretroviral treatment.
There was progressive confusion, and the patient was then admitted three months later following a fall with head injury, and new right sided seizures.
At this point, CD4 count was 32.
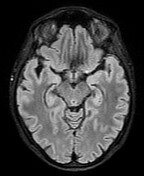
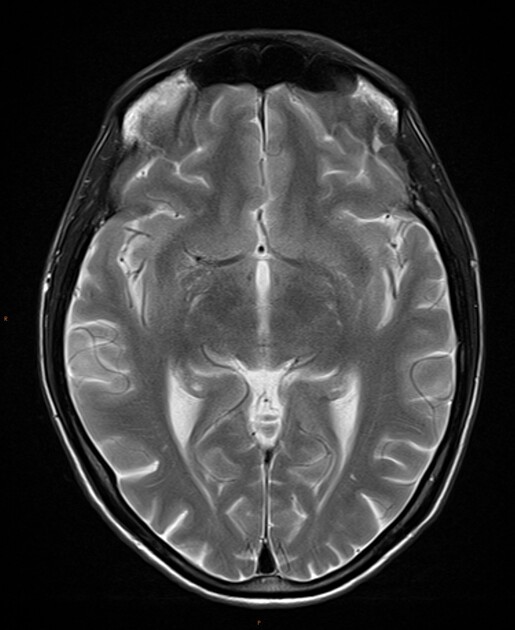
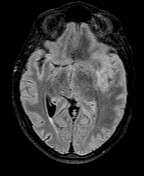
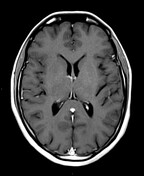
3/12 later, CD4 32, seizures




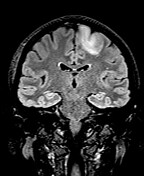

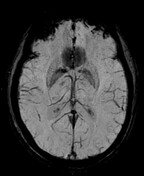




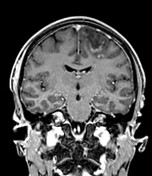

Progressive changes from the normal MRI three months ago.
Large region of signal abnormality around the left precentral and superior frontal sulci involving the white matter of the precentral gyrus and superior frontal gyri. There are further separate regions of abnormality in the left lateral frontal lobe and the right superior frontal gyrus. Within these regions there may also be some cortical involvement. There are a few new scattered subcortical abnormalities in the right corona radiata and the left posterior internal capsule, and enlargement of one of the pre-existing subcortical hyperintensities in the right frontal operculum. The other pre-existing hyperintensities remain nonspecific.
Around the margin of the largest lesion there are smaller punctate high T2W / low T1W cystic spaces, compared with the more diffuse increased T2W signal in the rest of the lesion. There is also new mixed linear and nodular enhancement, along a leading edge of the left frontal abnormality but also in the right gyral changes. Diffusion is predominantly facilitated in all sites of abnormality with some thin peripheral margins of lower ADC values, matching the enhancing tissues. No abnormal SWI signal.
There is a shallow subgaleal hematoma over the right occiput, with minor possible focal widening of the right lambdoid suture, but no appreciable skull fracture or intracranial traumatic abnormalities on CT or MRI.
Other than mild swelling of the left frontal region, parenchymal volume and CSF configuration remain stable. Normal major vascular signal voids are maintained.
The clinical and radiological situation favored an immune reconstitution inflammatory syndrome, with progressive multifocal leukoencephalopathy (PML-IRIS). However, repeat CSF analyzes for JC virus PCR were negative.
Within a few weeks, there was further neurological deterioration now with worsening right limb weakness and expressive speech disturbance.
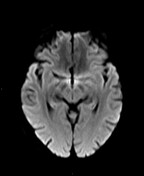
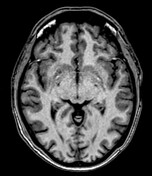
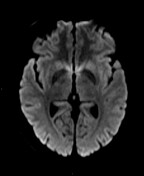
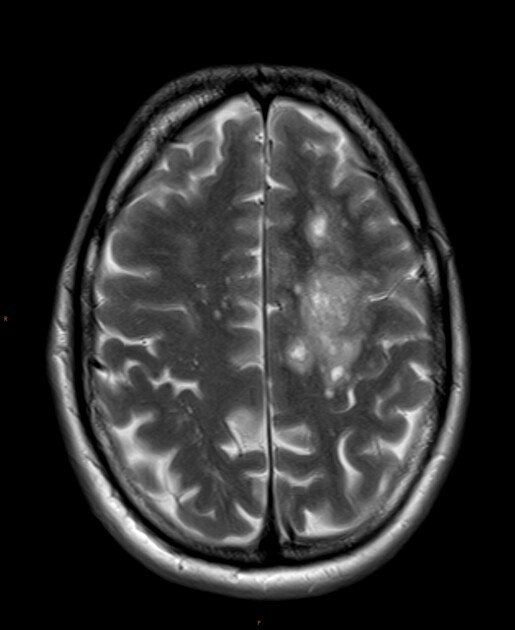
1/12 later, worse motor/speech





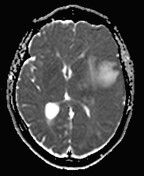

Significant radiological progression at all sites, with confluent expansile white matter abnormality, worsened enhancing foci, and progressive mass effect. Midline shift with left frontal subfalcine herniation, but no transtentorial shift.
Given the clinical deterioration and to support ongoing management, the patient was transferred to a tertiary center for brain biopsy. This was taken from the left precentral gyrus consistent with the worst focus of disease.
Brain biopsy PCR was positive for JC virus at 361 MIU/mL (8.56 log copies / mL), and repeat CSF analysis of 0.2 MIU/mL (3.37 log copies / mL).
Microscopy of the biopsy showed hypercellular brain parenchyma. Large pleomorphic astrocytes, some multinucleated, and oligodendroglial cells with eosinophilic glass inclusions. Perivascular aggregate lymphocytes also present. CD3 positive T cells and CD20 positive B cells were present on immunohistochemistry, as well as CD68 macrophages. SV40 staining for JC virus was also positive. Reactive GFAP, p53 and MIB1 staining, with negative IDH1 and maintained ATRX.
These findings were all compatible with progressive multifocal leukoencephalopathy.
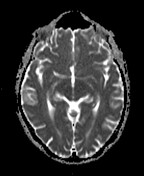
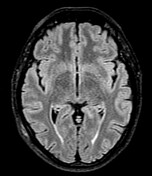
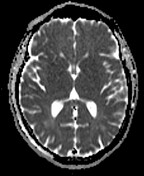
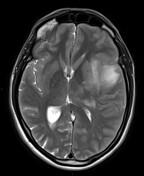
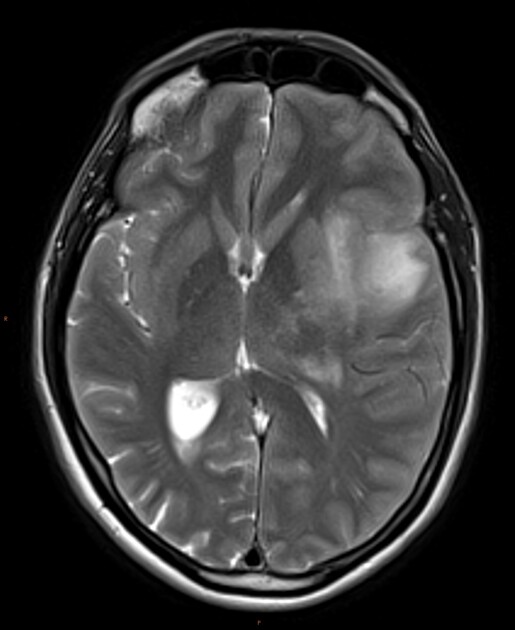
One year following Tx


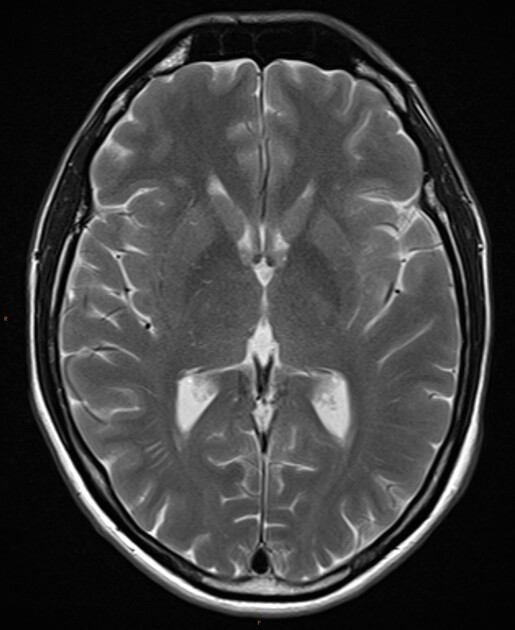
Following confirmation of PML high dose steroids were commenced, with good neurological and imaging response. Imaging one year following brain biopsy shows continued response to treatment (continued antiretroviral and low dose systemic steroids).
Case Discussion
PML-IRIS is a rare neuroinflammatory condition, typically seen in patients undergoing treatment for HIV / AIDS, or on natalizumab for multiple sclerosis.
The features can exacerbate pre-existing PML with immune reconstitution (PML-d-IRIS), or have simultaneous development with inflammation as seen in this case (PML-s-IRIS).
The features suggesting IRIS includes the enhancing pattern and the progressive mass effect (both atypical for PML).
Reaching confirmation of JC virus infection through CSF or direct brain analysis are required in these cases to allow commencement of steroids, which would otherwise worsening immune status and allow unfettered progression of other opportunistic infections.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.