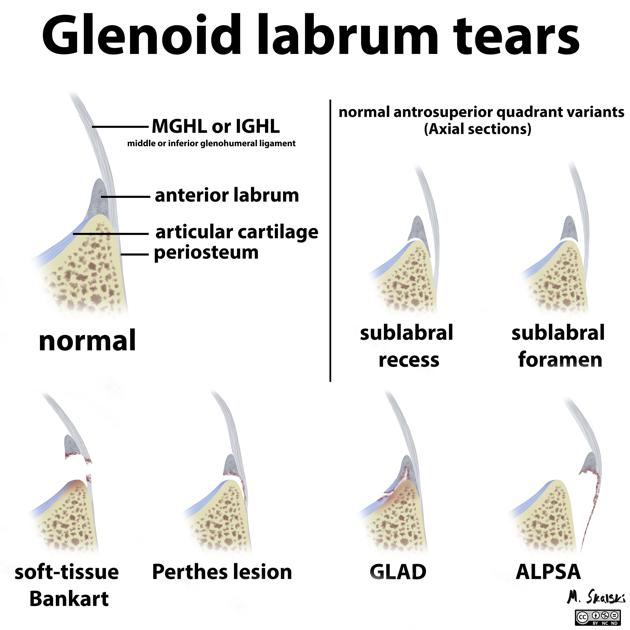
An anterior labroligamentous periosteal sleeve avulsion (ALPSA) lesion is similar to a Bankart lesion, in that it too is usually due to anterior shoulder dislocation and involves the anterior inferior labrum.
On this page:
Epidemiology
It is often the result of chronic injury rather than acute dislocation; the incidence of ALPSA lesions increases in patients with multiple dislocations.
Pathology
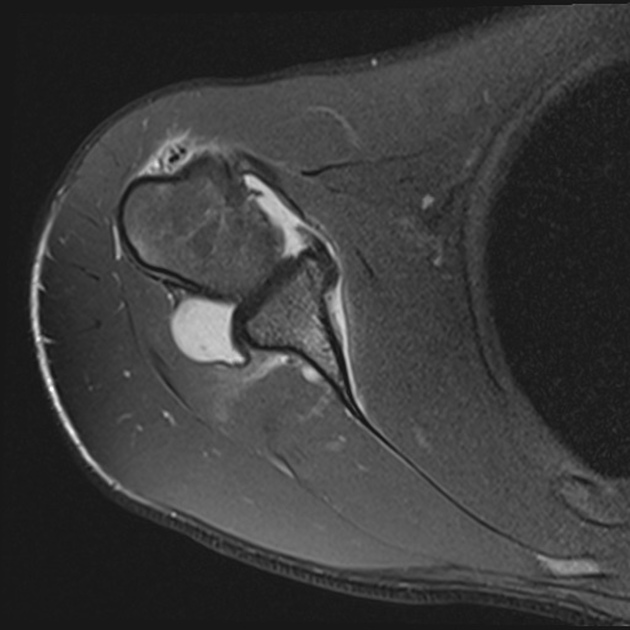
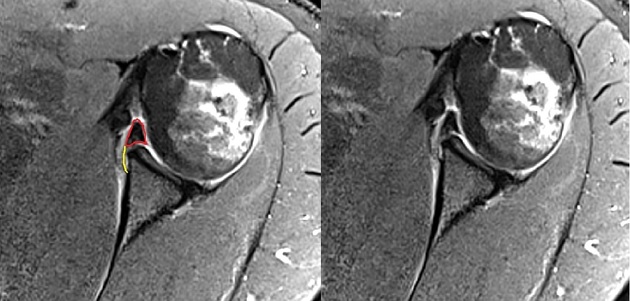
An ALPSA lesion refers to a detachment of the anteroinferior labrum from the glenoid. The scapular periosteum is unruptured but widely lifted or stripped. The labrum remains attached to the periosteum and can rotate medially to a position along the anterior surface of the scapular neck.
Radiographic features
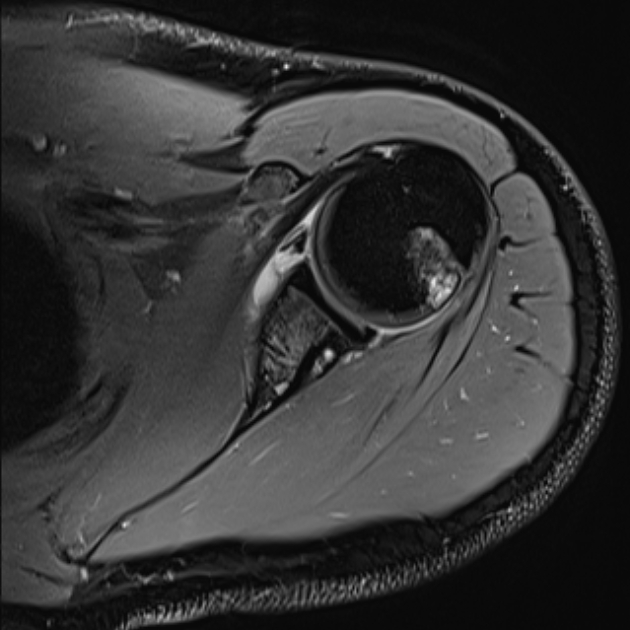
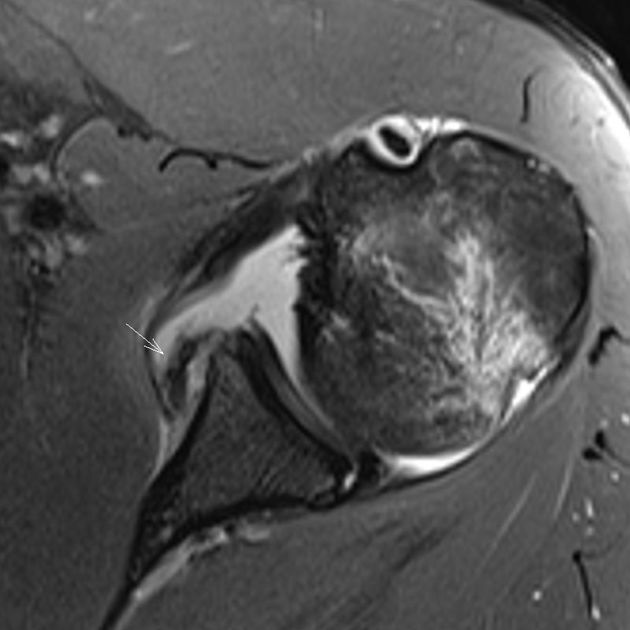
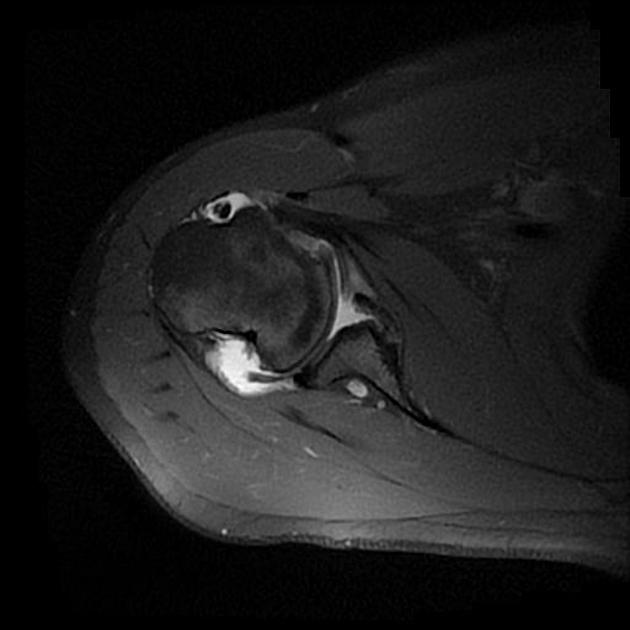
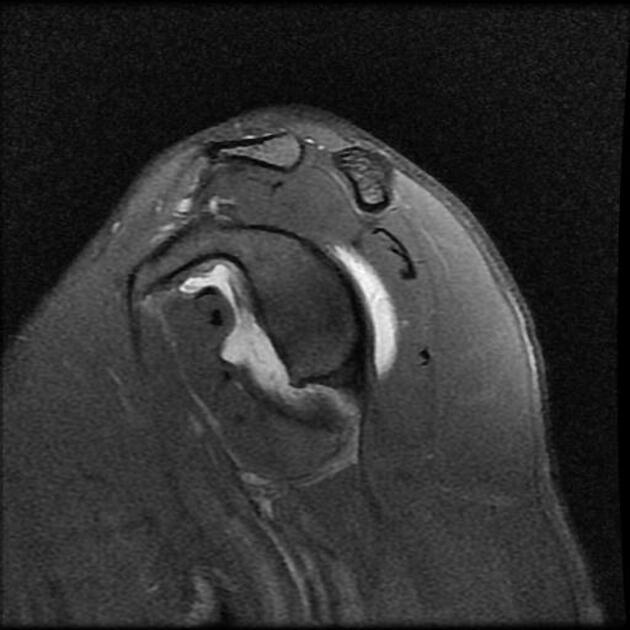
MRI
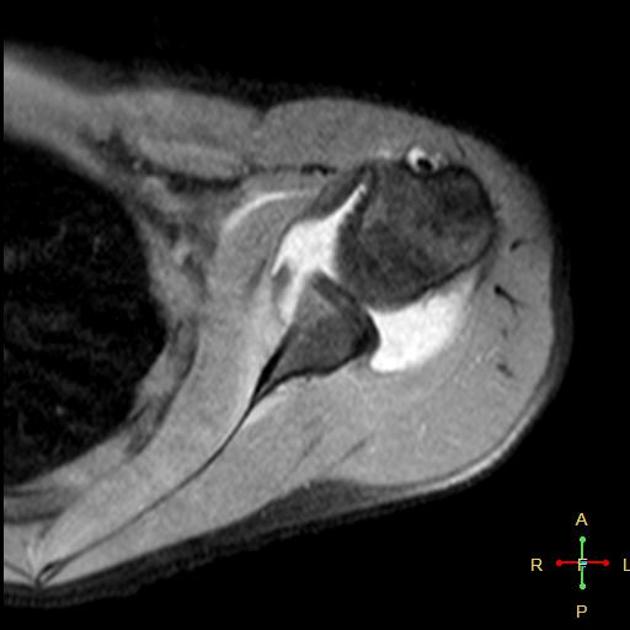
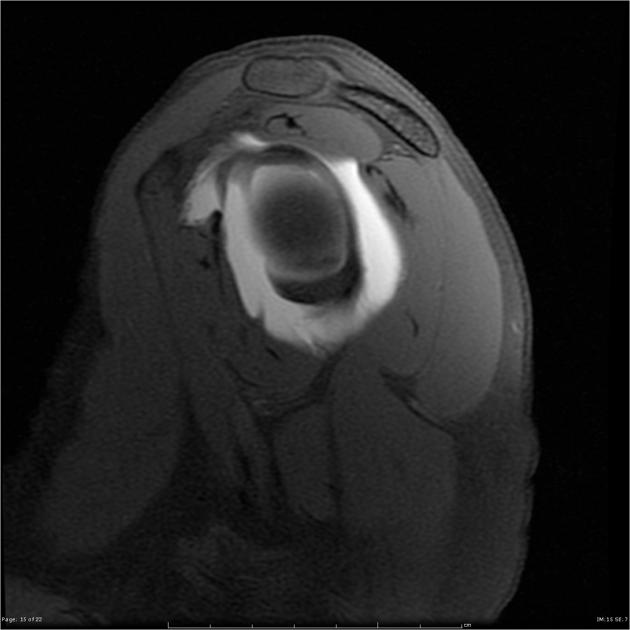
The clue to identifying an ALPSA lesion is the medial displacement and inferior shifting of the inferior glenohumeral ligament (IGHL) complex. A Hill-Sachs defect may be seen in association.
MR arthrography
May show contrast material entering a cleft between the anteroinferior glenoid and the labrum. The labral tissue is detached with the periosteal attachment stripped without tearing.
Treatment and prognosis
Unlike the Bankart lesion in which the labrum and glenoid periosteum are avulsed from the underlying glenoid, an ALPSA lesion involves mobilisation of the labrum which remains attached to the periosteum overlying the glenoid (thus sleeve). As a result, an ALPSA lesion may heal (as opposed to a Bankart lesion which does not), however it can do so in an abnormal position requiring identification and early surgical repair.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.