The Bethesda system for reporting thyroid cytopathology comprises six categories of pathological reporting of thyroid FNA, with each category linked to a malignancy risk.
On this page:
Usage
The Bethesda system was first published in 2010 and has been revised twice, with the most recent and third edition published in 2023 to align with the 2022 WHO classification of thyroid tumours 3.
Classification
The adult diagnostic categories for the 2023 Bethesda system are as follows 4:
-
category I
-
non-diagnostic
cyst fluid only
virtually acellular special
other, e.g. obscuring blood, clotting artifact, drying artifact
risk of malignancy ~13% (range 5-20%)
usual management: repeat US-guided thyroid FNA (which will be diagnostic in ~70% (range 60-80%) of cases)
-
-
category II
-
benign
consistent with follicular nodular disease (includes adenomatoid nodule, colloid nodule, etc.)
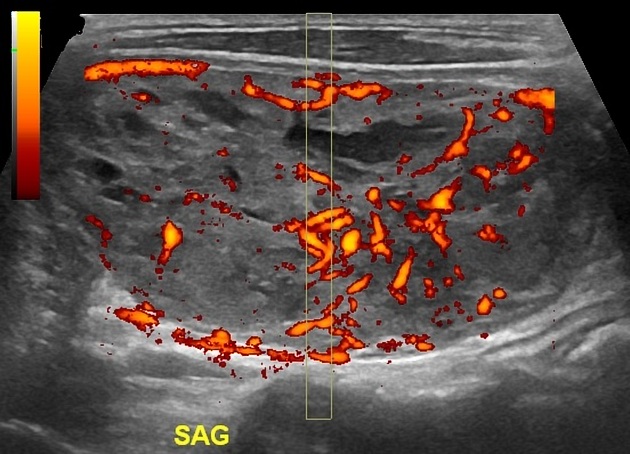
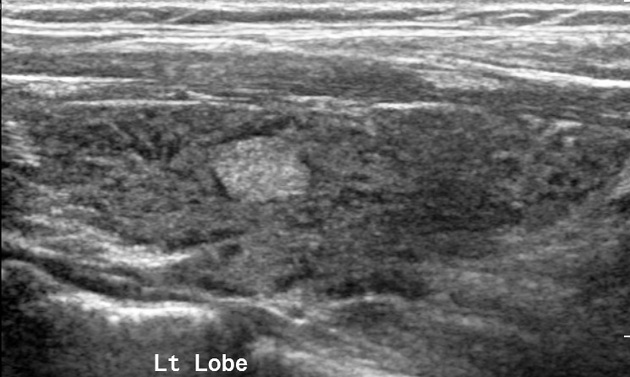
consistent with chronic lymphocytic (Hashimoto) thyroiditis in the proper clinical context
consistent with granulomatous (subacute) thyroiditis
risk of malignancy: ~4% (range 2-7%)
usual management: clinical and ultrasound follow-up
-
-
category III
atypia of undetermined significance; specify AUS-nuclear atypia or AUS-other
risk of malignancy: ~22% (range 13-30%)
usual management: repeat US-guided FNA, molecular testing (if available), diagnostic hemithyroidectomy, or surveillance
-
category IV
follicular neoplasm;specify if oncocytic (Hürthle cell) type
risk of malignancy: ~30% (range 23-34%)
usual management: molecular testing (if available), diagnostic hemithyroidectomy
-
category V
suspicious for suspicious for malignancy (e.g. papillary thyroid carcinoma, medullary thyroid carcinoma, metastatic carcinoma, lymphoma)
risk of malignancy: ~74% (range 67-83%)
usual management: molecular testing (if available), hemithyroidectomy/thyroidectomy
-
category VI
-
malignant
papillary thyroid carcinoma
medullary thyroid carcinoma
squamous cell carcinoma
carcinoma with mixed features (specify)
metastatic malignancy
non-Hodgkin lymphoma
risk of malignancy: ~97% (range 97-100%)
usual management: hemithyroidectomy/thyroidectomy
-




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.