Carpal tunnel syndrome results from compression of the median nerve (tunnel syndrome) within the carpal tunnel. It is a cause of significant disability and is the most prevalent of the three common median nerve entrapment syndromes, the other two being anterior interosseous nerve syndrome and pronator teres syndrome.
On this page:
Epidemiology
The prevalence of carpal tunnel syndrome is estimated to be ~5% (range 3-6%) of the global adult 22,24, with a lifetime incidence of 10-16%, depending on occupational risk 4.
Carpal tunnel syndrome is most common in the early fifties with a second peak in the 75-84-year age group 26. It is more common in women 26. Carpal tunnel syndrome is uncommon in children 26.
Risk factors
Risk factors for carpal tunnel syndrome include 18,20:
pregnancy: most common in the third trimester and usually resolves post-partum 26
Diagnosis
There are no established diagnostic criteria for carpal tunnel syndrome, and reliance on one diagnostic parameter is not recommended 26. Helpful tools include validated questionnaires (e.g. Kamath and Stothard questionnaire, Katz and Stirrat hand symptom diagram), clinical examination, nerve conduction studies, and imaging 26.
Clinical presentation
Carpal tunnel syndrome is primarily defined by pain and sensory symptoms:
brachialgia paraesthetica nocturna, or nocturnal ascending pain emanating from the wrist, is typical
sensory symptoms affect the first three digits and, depending on innervation patterns, the radial aspect of the fourth digit
positive Tinel test: paraesthesias elicited by tapping the median nerve at the wrist
positive Phalen test: paraesthesias caused by wrist flexion over 30-60°
Hand weakness, as a rule, is a late symptom 5.
The dominant hand is affected more frequently, and bilateral involvement has been reported to occur in ~30% (range 8-50%) of cases.
The clinical presentation can harbour some pitfalls. Sensory and pain symptoms of the pronator teres syndrome (PTS) and carpal tunnel syndrome can overlap; one can distinguish the two by examining for numbness of the forearm, which does not occur in carpal tunnel syndrome and ask about nocturnal exacerbation, which is atypical in PTS. Provocation tests as detailed above can help further.
Pathology
The pathogenesis of carpal tunnel syndrome has yet to be fully elucidated but is thought to related to increased carpal tunnel pressure causing ischaemic compression of the median nerve and local demyelination 20,21,24. Decreased carpal tunnel volume plays a role 26. Scarring can result in median nerve adhesion 20,24. Sensory fibres are typically first affected, followed by motor fibres 21.
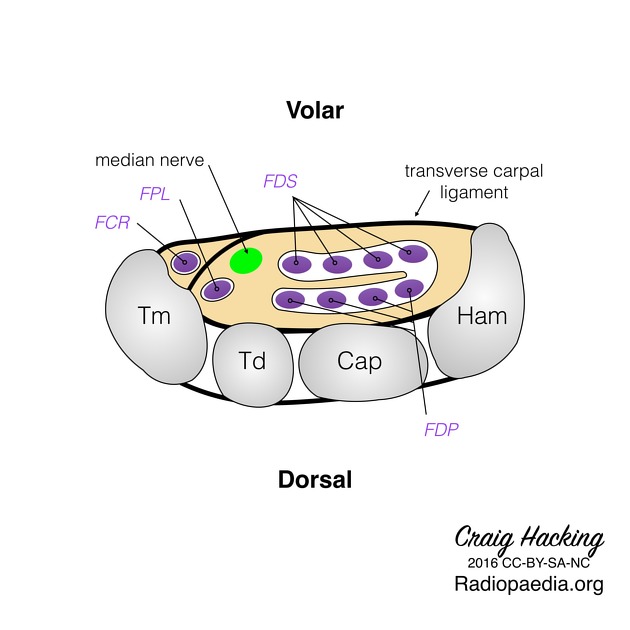
Compression can occur at the proximal aspect of the flexor retinaculum or at the level of the hook of hamate 20,22.
Aetiology
There is a wide range of causes of carpal tunnel syndrome:
-
mechnical
work-related wrist overuse in jobs with increased wrist flexion/extension angular velocities, e.g. cleaning, laundry, slaughterhouse jobs, result in increased carpal tunnel pressure 18,20
-
space occupying lesions
bifid median nerve due to increased cross-sectional area 14
mass, e.g. ganglion cyst, peripheral nerve sheath tumour 22
aberrant muscle bellies, most commonly of the lumbricals or index finger flexor digitorum superficialis 19
osteoarthritis 22,26
-
traumatic
trauma, e.g. post distal radius or wrist fracture, lunate dislocation, can cause acute carpal tunnel syndrome 18,22,23,26
-
inflammatory
flexor tendon tenosynovitis, e.g. in rheumatoid arthritis 20
hormonal: related to increased fluid contents, e.g. pregnancy, obesity, renal failure, hypothyroidism, menopause, oral contraceptive pill, heart failure 22,26
-
neuropathy
diabetic neuropathy 22
hereditary neuropathy (rare) 26
-
rare causes
lysosomal storage disorders: mucopolysaccharidosis type I is the most common cause in children 26
amyloidosis: carpal tunnel syndrome may precede other manifestations by many years 26
acromegaly 26
Associations
cervical radiculopathy 20
brachial plexopathy 20
Radiographic features
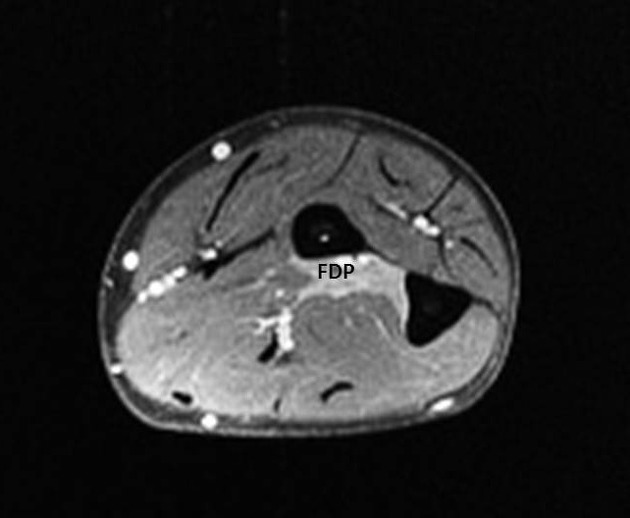
Ultrasound and MRI are the two imaging modalities that best lend themselves to investigating entrapment syndromes. Next to directly visualising direct causes and anatomical variants (e.g. a Gantzer muscle), recognising pathological muscle signal patterns on MRI can point to the affected nerve.
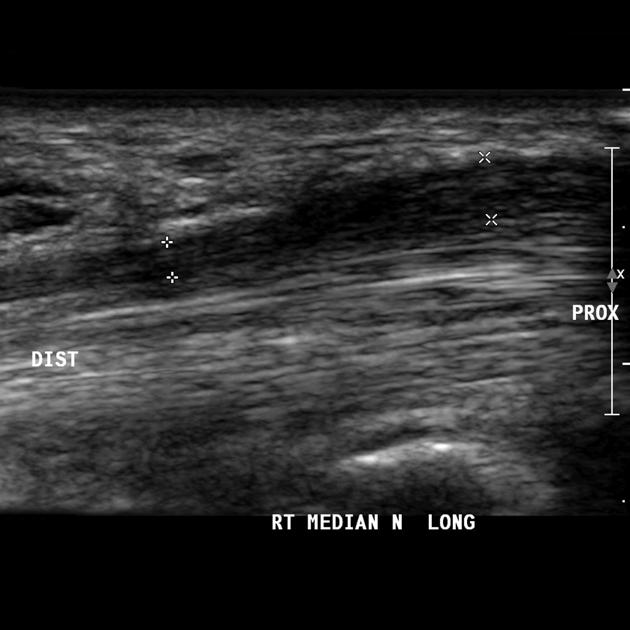
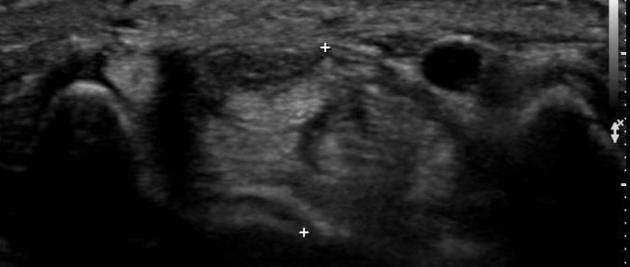
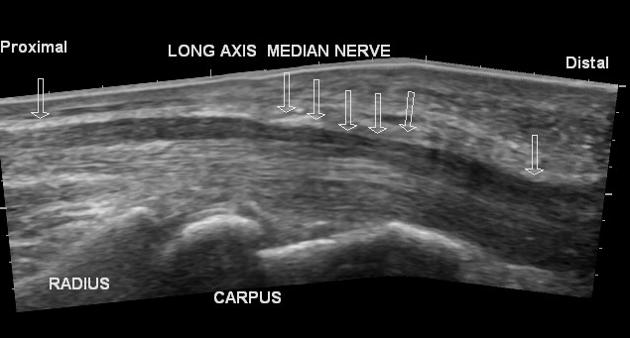
Ultrasound
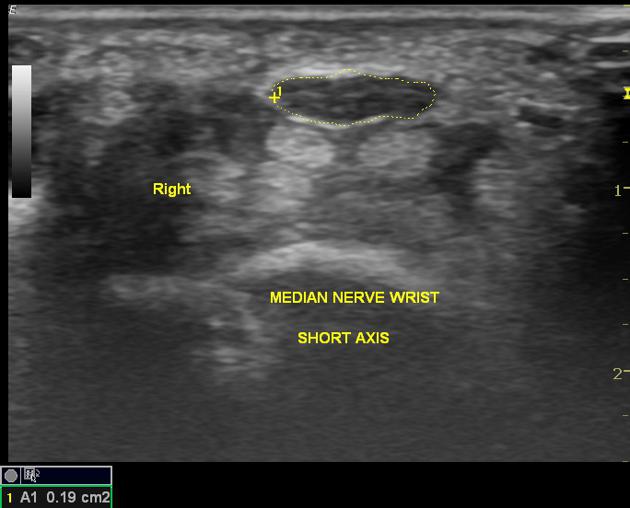
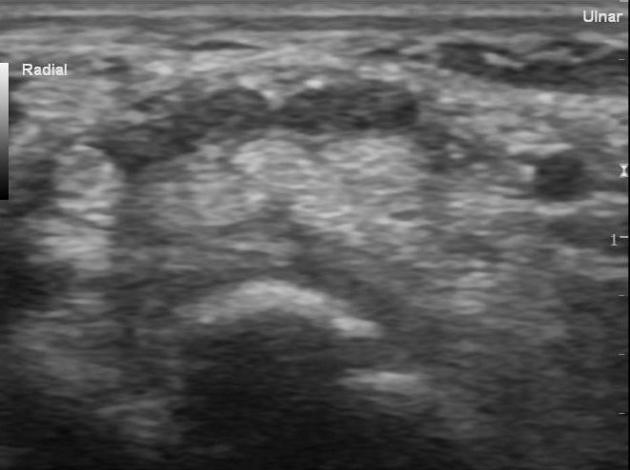
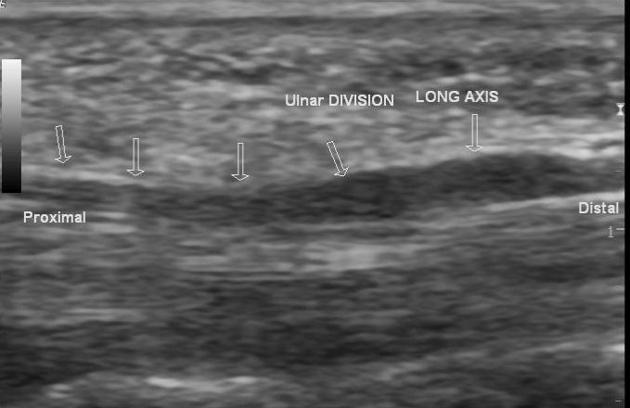
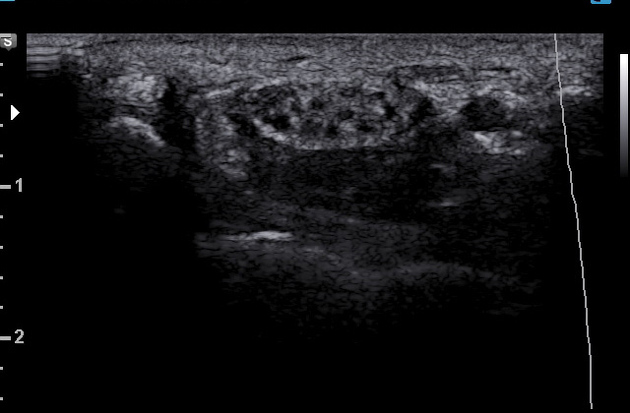
In imaging median nerve syndromes, ultrasound is useful in examining carpal tunnel syndrome, potentially revealing, in fully developed cases, a triad of:
palmar bowing of the flexor retinaculum (>2 mm beyond a line connecting the pisiform and the scaphoid)
distal flattening of the nerve
enlargement of the nerve proximal to the flexor retinaculum
Enlargement of the nerve seems to be the most sensitive and specific criterion, but what cut-off value for pathological size remains debated; the normal cross-sectional area (CSA) is given at 9-11 mm2 (0.09-0.11 cm2), but the range of CSAs deemed pathological is wide. According to one study, a 2 mm2 difference in nerve CSA between the level of the pronator quadratus and the carpal tunnel has a 99% sensitivity and 100% specificity for carpal tunnel syndrome 9.
Intraneural hyper-vascularisation is another feature with high diagnostic accuracy, although may be absent in chronic cases 16,17.
Some of the other proposed findings include ref:
flattening ratio of over 3 times
bowing of the flexor retinaculum of >4 mm
If a bifid median nerve is present, measuring the combined cross-sectional area can be performed with an increase in cross-sectional area of ≥4 mm2 between the median nerve at the proximal-third pronator quadratus level and in the carpal tunnel providing >90% sensitivity/specificity for carpal tunnel syndrome 15.
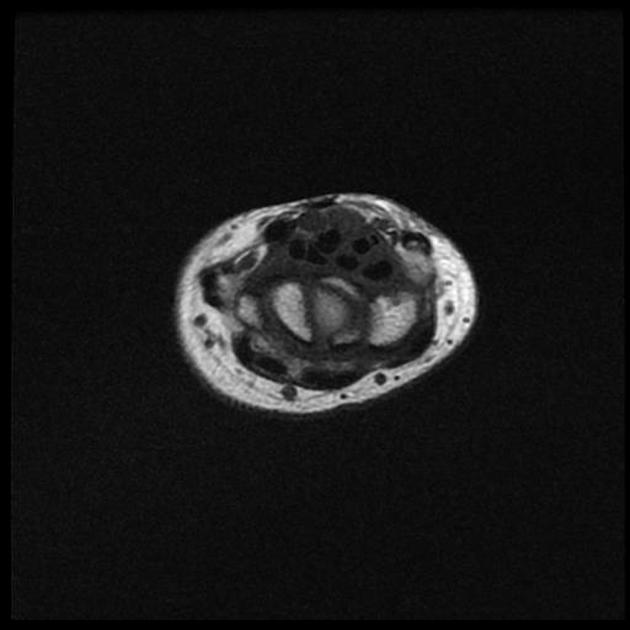
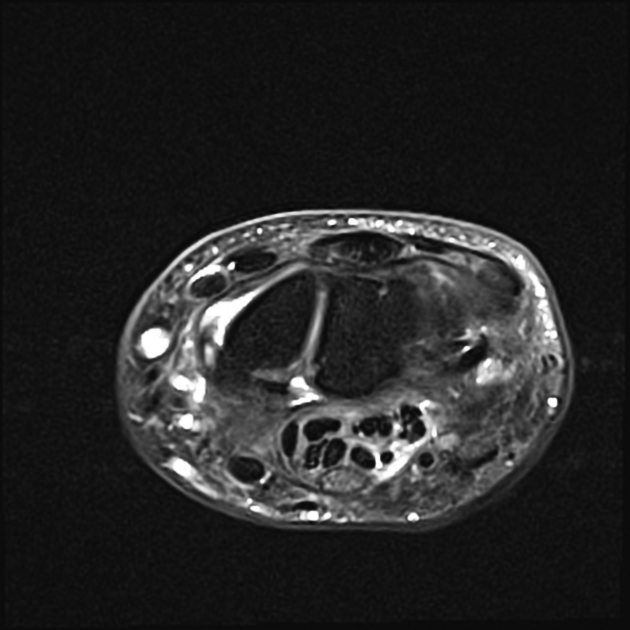
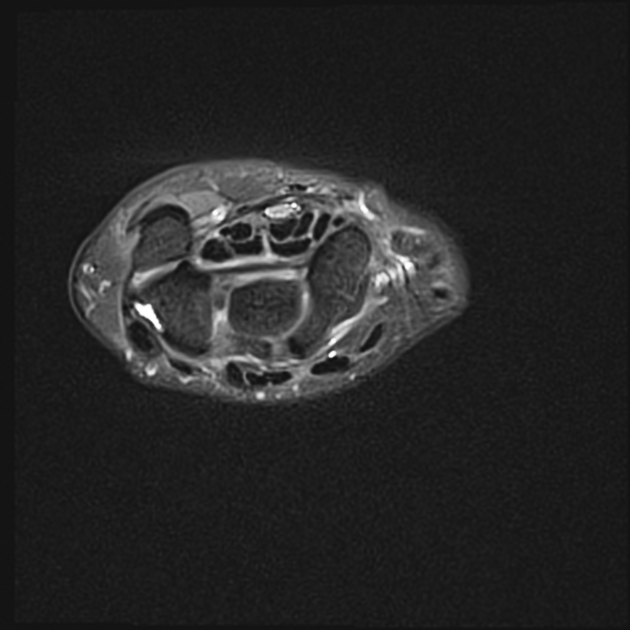
MRI
MRI has good-to-excellent sensitivity (84-100%) and specificity (85-94%) for diagnosing carpal tunnel syndrome when using cross-sectional area >15 mm2 as a cut-off 12,13. MRI is especially well-suited for detecting masses, arthritic changes, and normal variants (e.g. bifid median nerve) 5.
In carpal tunnel syndrome, MRI can demonstrate 4:
palmar bowing of the flexor retinaculum
nerve thickening at the carpal tunnel inlet (level of the pisiform)
nerve flattening at the carpal tunnel outlet (level of the hook of hamate)
-
increased cross-sectional area
ultrasound values do not correlate with MRI values 11
>15 mm2 at the carpal tunnel inlet or outlet can be used as a diagnostic criterion or cut-off 12,13
>19 mm2 has been proposed as a marker for severe carpal tunnel syndrome 13
oedema or loss of fat within the carpal tunnel
neural oedema +/- contrast enhancement
Treatment and prognosis
Carpal tunnel syndrome is initially often treated conservatively with splinting, physiotherapy, and/or non-steroidal anti-inflammatory drugs (NSAIDs) 24,26.
Corticosteroid injections into the carpal tunnel can alleviate symptoms. Ultrasound-guided perineural injections of steroid result in improved symptoms and function from either pharmacological effects or less likely the mechanical effect of hydrodissection 24 although long-term (>6 months) effectiveness is not clear 26. Higher dose steroids (e.g. triaminolone 80 mg) show better effects than lower dose steroids (e.g. triaminolone 80 mg) 24,25.
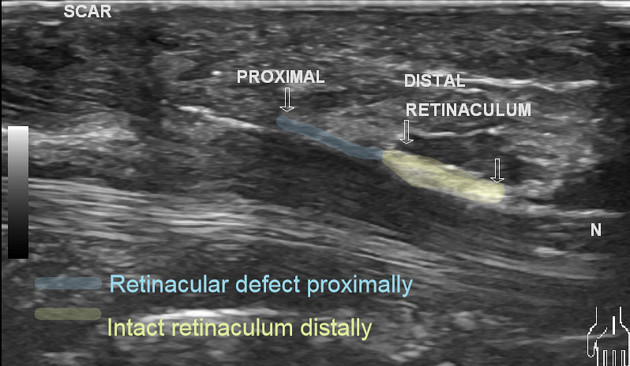
Surgical release of the flexor retinaculum is indicated in cases of pronounced nocturnal pain, permanent dysaesthesias and prolonged distal motor latency on nerve conduction studies (>6 ms) ref. Most (~75%) patients have an excellent outcome from surgery, although ~10% have worsening symptoms, and ~10% undergo revision surgery 24,26. This surgery may be open or ultrasound-guided percutaneous 24,26.
Complications
recurrent carpal tunnel syndrome (i.e. failed carpal tunnel release)
median nerve injury: very rare 10
Differential diagnosis
Possible differential diagnoses of carpal tunnel syndrome include:











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.