Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)
Updates to Synonym Attributes
Updates to Synonym Attributes
Updates to Article Attributes
Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy (CADASIL) is an autosomal dominant microvasculopathy, characterised by recurrent lacunar and subcortical white matter ischaemic strokes and vascular dementia in young and middle age patients without known vascular risk factors. There is disproportionate cortical hypometabolism.
Epidemiology
CADASIL is an autosomal dominant trait, with patients typically becoming symptomatic in adulthood (30-50 years of age).
Clinical presentation
Presentation is usually with recurrent transient ischaemic attacks (TIAs) or strokes in multiple vascular territories. Presenile dementia and migraines develop in the third-to-fourth decades of life. Clinically, CADASIL often has a similar presentation as migraines and may also have auras. Depression, psychosis, pseudobulbar palsy and focal neurological defects as well as seizures are also seen 2,3.
Pathology
CADASIL results from a mutation on chromosome 19q12 involving the Notch 3NOTCH3 gene, and as the name implies is inherited as an autosomal dominant trait. It results in small vessel and arteriole stenosis secondary to fibrotic thickening of the basement membrane of the vessels.
Histology
An angiopathy of small and middle sized arteries is characteristic, without atherosclerosis or amyloid deposition 3. Diagnosis requires genetic identification of the mutated gene 4.
Radiographic features
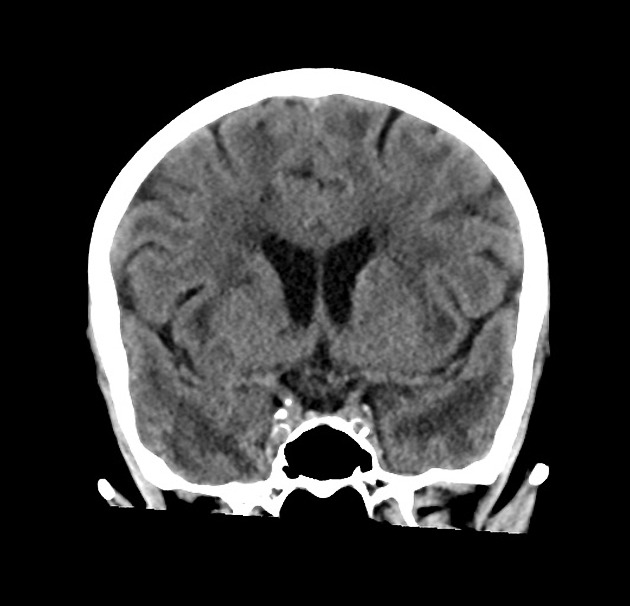
CT
CT is non-specific, demonstrating white matter regions of low attenuation.
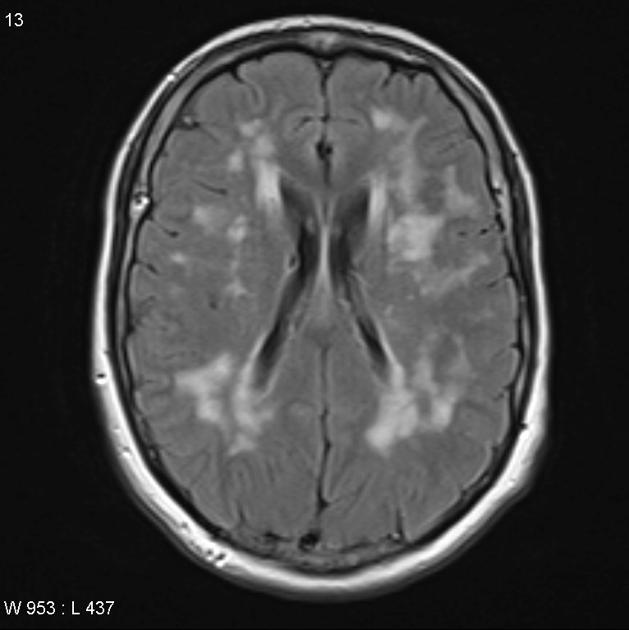
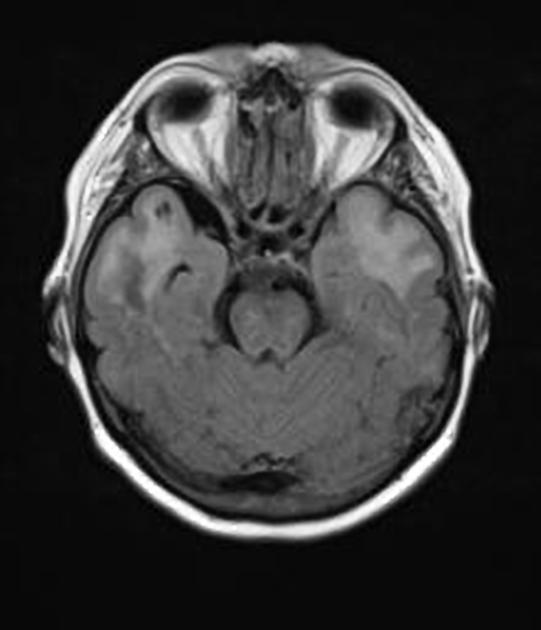
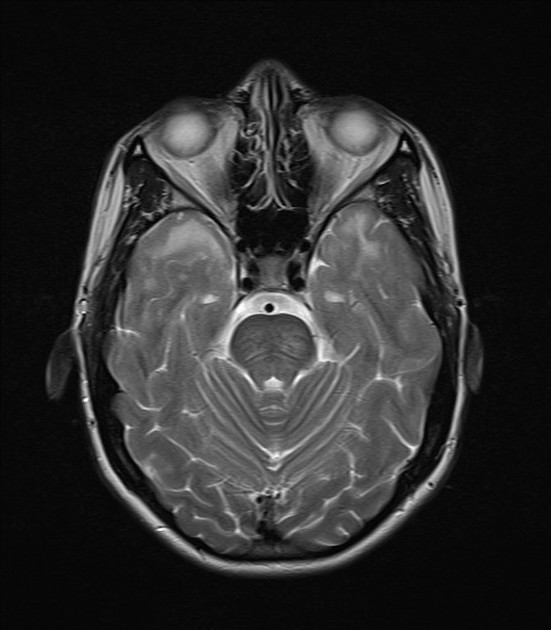
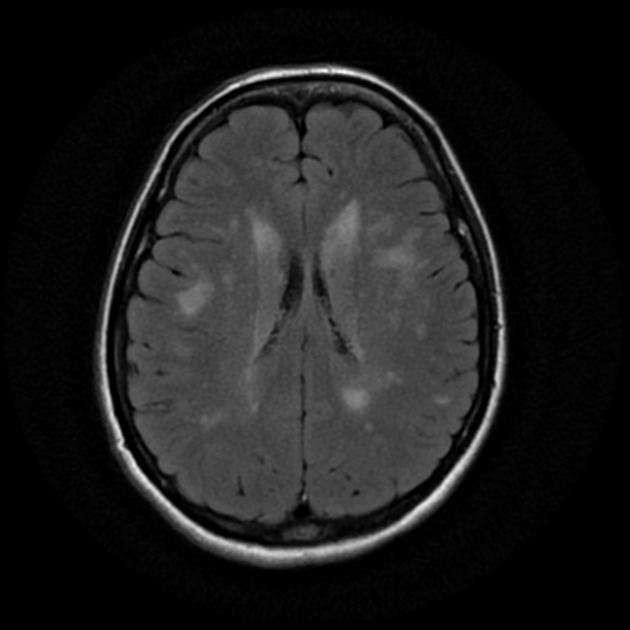
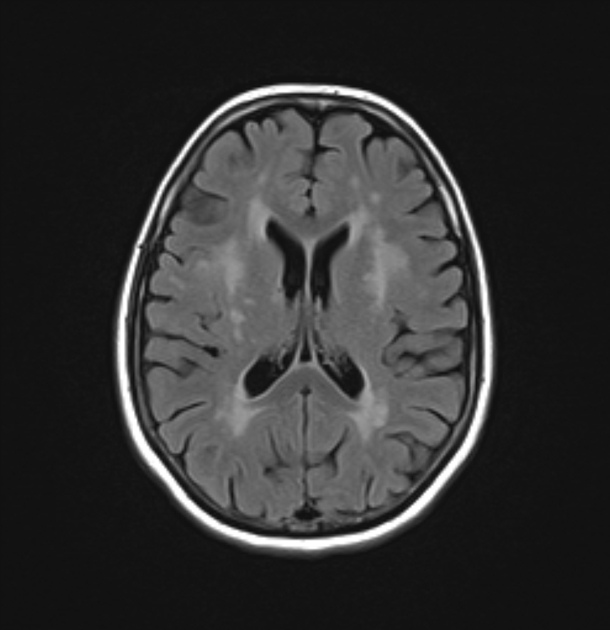
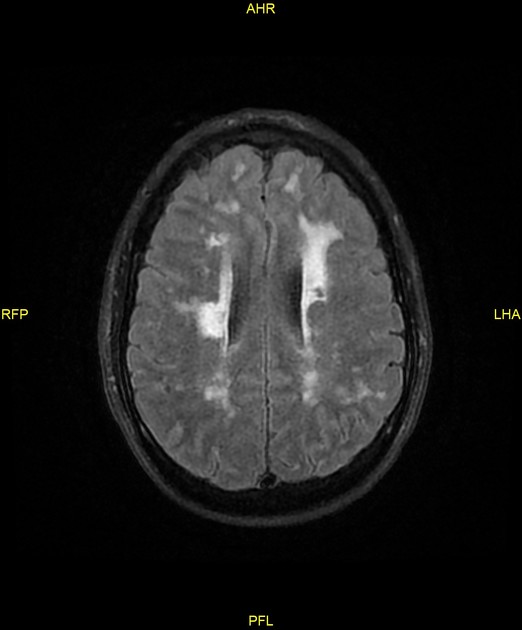
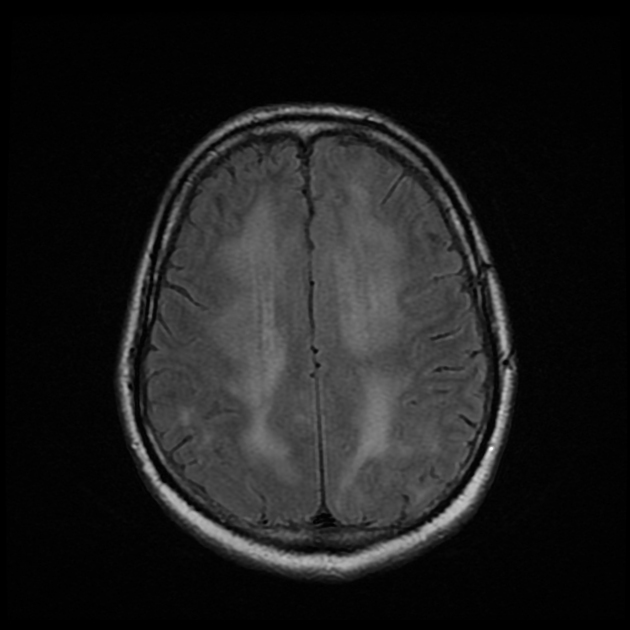
MRI
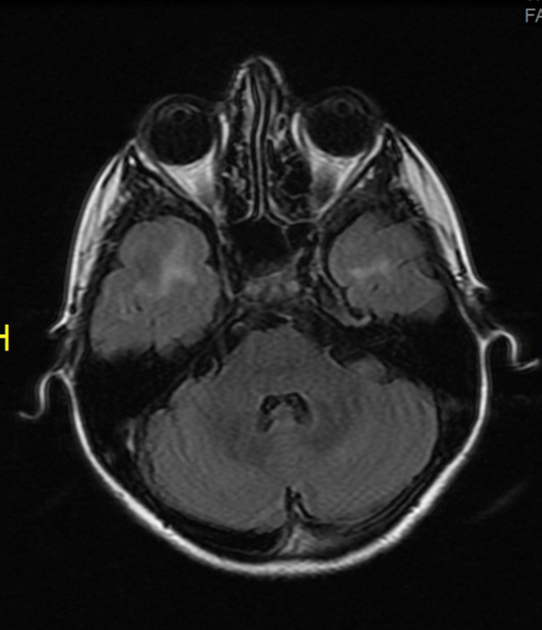
MRI is the investigation of choice, often demonstrating widespread confluent white matter hyperintensities 2. More circumscribed hyperintense lesions are also seen in the basal ganglia, thalamus and pons 3.
Although the subcortical white matter can be diffusely involved, in the initial course of the disease involvement of the anterior temporal lobe (86%) and external capsule (93%) are classical 2. There is relative sparing of the occipital and orbitofrontal subcortical white matter 2, subcortical U-fibers and cortex 3.
Cerebral microhaemorrhages have been reported to occur in ~45% (range 25-70%) of cases without a characteristic distribution 1.
Eventually cerebral atrophy ensues, which correlates well with the degree of cognitive decline.
Treatment and prognosis
Typically the disease has a variable but progressive course leading to death between 50-70 years of age 2,4.
Differential diagnosis
General imaging differential considerations include:
- multiple early age infarcts from a hypercoagulable state
- MELAS
- subcortical arteriosclerotic encephalopathy (SAE)
- Susac syndrome
- CNS vasculitis
- COL4A1 brain small-vessel disease
Practical points
- think of it in younger patients with small vessel ischaemic white matter change
- predilection for anterior temporal lobe white matter is a distinctive feature
- sparing of the cortex and subcortical U-fibres is typical
See also
Image ( create )
Image 7 MRI (Ax T2 Flair PROP) ( create )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.