Staging of cervical cancer can either be based on the TNM or FIGO system.
Classification
Revised FIGO staging of cervical carcinoma (2018)
- FIGO no longer includes stage 0 (Tis)
-
I: confined to cervix uteri (extension to the corpus should be disregarded)
-
IA: invasive carcinoma only diagnosed by microscopy
- IA1: stromal invasion <3 mm in depth
- IA2: stromal invasion ≥3 mm and <5 mm in depth
-
IB: invasive carcinoma with measured deepest invasion ≥5 mm (greater than stage IA), lesion limited to the cervix uteri
- IB1: invasive carcinoma ≥5 mm depth of stromal invasion and <2 cm in greatest dimension
- IB2: invasive carcinoma ≥2 cm and <4 cm in greatest dimension
- IB3: invasive carcinoma ≥4 cm in greatest dimension
-
IA: invasive carcinoma only diagnosed by microscopy
-
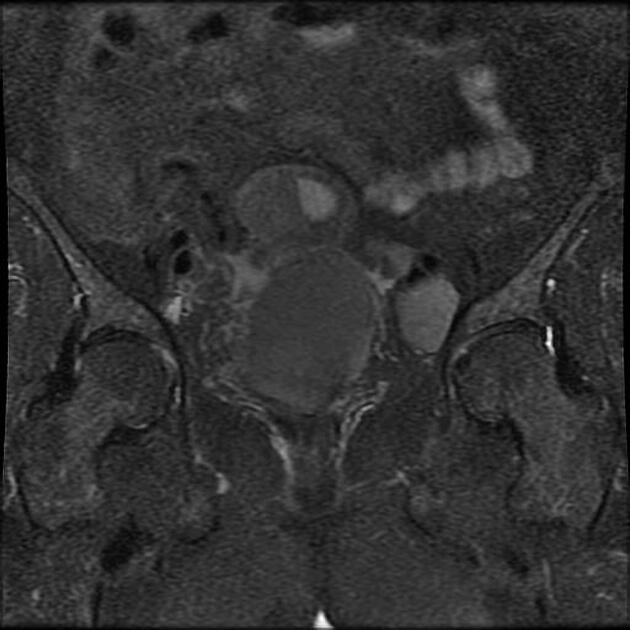
II: beyond the uterus, but has not extended onto the lower third of the vagina or to the pelvic wall
-
IIA: involvement limited to the upper 2/3 of vagina without parametrial invasion
- IIA1: invasive carcinoma <4 cm in greatest dimension
- IIA2: invasive carcinoma ≥4 cm in greatest dimension
- IIB: with parametrial involvement but not up to the pelvic wall
-
IIA: involvement limited to the upper 2/3 of vagina without parametrial invasion
-
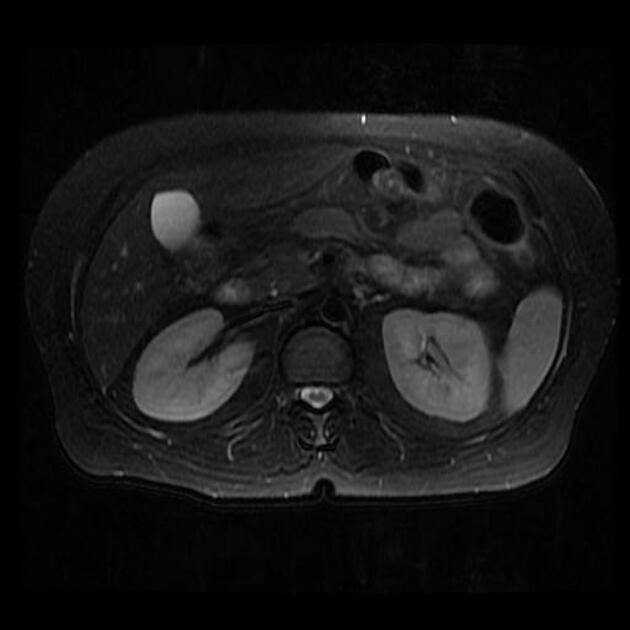
III: carcinoma involves the lower third of the vagina and/or extends to the pelvic wall and/or causes hydronephrosis or non‐functioning kidney and/or involves pelvic and/or paraaortic lymph nodes
- IIIA: carcinoma involves the lower third of the vagina, with no extension to the pelvic wall
- IIIB: extension to the pelvic wall and/or hydronephrosis or non‐functioning kidney (unless known to be due to another cause)
-
IIIC: involvement of pelvic and/or para-aortic lymph nodes, irrespective of tumour size and extent
- IIIC1: pelvic lymph node metastasis only
- IIIC2: para-aortic lymph node metastasis
- with r (imaging) and p (pathology) notations to indicate how lymph nodes were identified
-
IV: carcinoma has extended beyond the true pelvis or has involved (biopsy-proven) the mucosa of the bladder or rectum (bullous oedema, as such, does not permit a case to be allotted to stage IV)
- IVA: spread to adjacent organs
- IVB: spread to distant organs 8
TNM Staging 2021 (AJCC version 9)
Primary tumour (T)
- Tx: primary tumour cannot be assessed
- T0: no evidence of primary tumour
- Tis: carcinoma in situ (cis)
-
T1: cervical carcinoma confined to the uterus (extension to the corpus should be disregarded)
- T1a: invasive carcinoma diagnosed only by microscopy (depth of invasion < 5 mm)11
- T1b: clinically visible lesion confined to the cervix
-
T2: cervical carcinoma invades beyond uterus but not to pelvic wall or to lower third of vagina
- T2a: tumour without parametrial invasion
- T2b: tumour with parametrial invasion
-
T3: tumour extends to pelvic wall and/or involves lower third of vagina, and/or causes hydronephrosis
- T3a: tumour involves lower third of vagina, no extension to pelvic wall
- T3b: tumour extends to pelvic wall and/or causes hydronephrosis or nonfunctioning kidney (unless known to be due to another cause)
- T4: tumour invades the mucosa of bladder or rectum, and/or extends beyond true pelvis 11
Regional lymph nodes (N)
- Nx: regional lymph nodes cannot be assessed
- N0: no regional lymph nodes metastasis
- N1: regional lymph node metastases to pelvic lymph nodes only
- N2: regional lymph node metastasis to para-aortic lymph nodes, with or without positive pelvic lymph nodes 11
Distant metastasis (M)
- M0: no distant metastasis
- M1: distant metastasis (includes metastasis to inguinal lymph nodes, intraperitoneal disease, lung, liver, or bone; excludes metastasis to pelvic or para-aortic lymph nodes or vagina) 11







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.