Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired demyelinating disease involving peripheral nerves, and is generally considered the chronic counterpart to Guillain-Barré syndrome (GBS).
On this page:
Epidemiology
CIDP is rare, with one systematic review finding an incidence rate of 0.33 per 100,000 person-years 10. It is slightly more common in males and is typically seen on an older adult demographic 10.
Clinical presentation
In typical CIDP, patients typically present with a subacute-to-chronic (>2 months) weakness of both proximal and distal musculature associated with areflexia and sensory changes 3. Rarely, in some patients, presentation can be acute and may closely mimic Guillain-Barré syndrome 2,4, known as acute-onset CIDP (A-CIDP).
In addition to the aforementioned typical presentation, many atypical variants of CIDP exist 7:
distal CIDP (distal acquired demyelinating symmetric (DADS) neuropathy)
multifocal CIDP (multifocal acquired demyelinating sensory and motor (MADSAM) neuropathy or Lewis-Sumner syndrome)
focal CIDP (chronic inflammatory demyelinating mononeuropathy (CIDM))
sensory CIDP (pure sensory CIDP)
motor CIDP (pure motor CIDP)
Pathology
Chronic inflammatory demyelinating polyneuropathy is an acquired demyelinating disease of the peripheral nervous system. Affected nerves demonstrate segmental infiltration with inflammatory cells (lymphocytes) and demyelination 4. Over time there is proliferation of Schwann cells and deposition of collagen resulting in thickening of the nerve and the characteristic onion bulb appearance 4. Involvement of the nerves results in changes of denervation in the supplied muscles 1.
Radiographic features
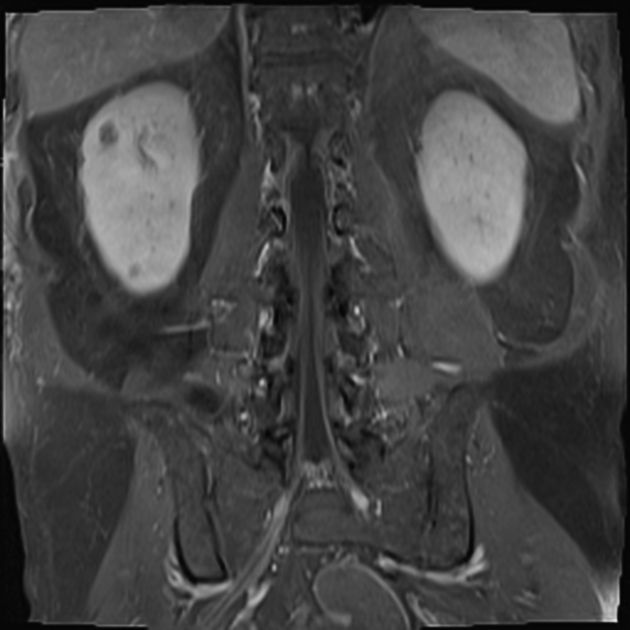
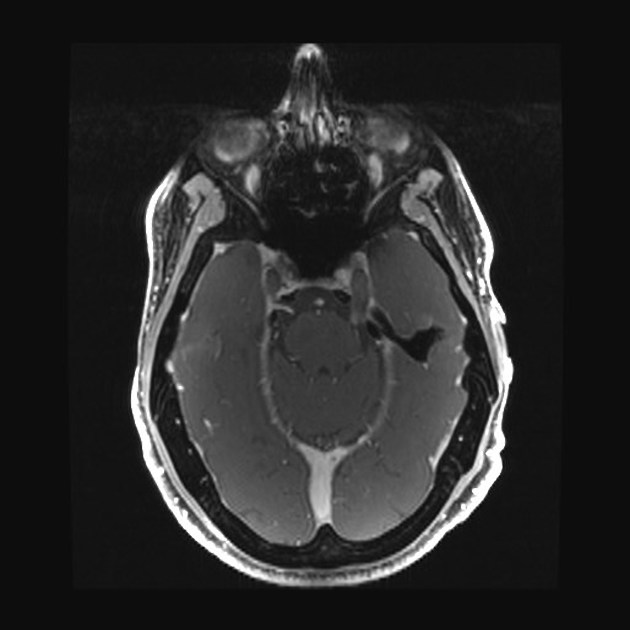
MRI
MRI is the modality of choice for imaging the changes of chronic inflammatory demyelinating polyneuropathy, the hallmark of which is thickening and enhancement of peripheral nerves, brachial and lumbosacral plexus and nerve roots. In many cases, the nerves become so thickened that they resemble onion bulbs. Approximately one-third of patients have cranial nerve involvement 5. Intercostal nerve involvement, although rare, has also been described 6.
In addition, the supplied muscles will demonstrate changes of denervation 1:
-
acute to subacute
diffuse increase in T2 signal
diffuse increased enhancement (seen best on fat suppressed T1 C+)
-
chronic
fatty atrophy
Treatment and prognosis
Chronic inflammatory demyelinating polyneuropathy can be treated with corticosteroids, intravenous immunoglobulin, plasmapheresis and other immunosuppression (e.g. rituximab, efgartigimod) 4,8,9.
Differential diagnosis
-
acute-onset CIDP (A-CIDP) can be similar
difficult to differentiate in the first 6 weeks
after 6-8 weeks GBS should be improving whereas CIDP will demonstrate chronic inflammation 2
chronic immune sensory polyradiculopathy (CISP)
autoimmune nodopathies and paranodopathies
hereditary neuropathies with late-onset (e.g. some types of Charcot-Marie-Tooth disease)






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.