Chronic thromboembolic pulmonary hypertension (CTEPH) is a distinct subgroup of pulmonary hypertension that most frequently develops following massive or repeated pulmonary embolism.
On this page:
Terminology
The term CTEPH should be used for patients with chronic thromboembolic disease and pulmonary hypertension as defined by a mean pulmonary arterial pressure (mPAP) ≥25 mmHg at rest determined by right heart catheterization. By contradistinction, chronic pulmonary emboli are mainly a consequence of incomplete resolution of pulmonary thromboembolism without pulmonary hypertension.
Epidemiology
Chronic thromboembolic pulmonary hypertension is a rare disease. The exact prevalence and annual incidence of CTEPH are unknown. Data from the United Kingdom suggest that CTEPH may occur in approximately five individuals per million population per year 2. A cumulative incidence of 0.1–9.1% within the first two years after an episode of symptomatic pulmonary embolus (PE) has been reported 3. However, some patients develop CTEPH in the absence of symptoms of previous acute PE 4.
Risk factors
history of pulmonary embolism
history of malignancy
splenectomy
chronic osteomyelitis
Clinical presentation
Clinical symptoms and signs are non-specific or absent in early stage of the disease, the impact of right heart failure only becomes evident in advanced disease. When present, the symptoms of CTEPH may resemble those of acute pulmonary embolism, idiopathic pulmonary arterial hypertension, asthma or chronic obstructive pulmonary disease 1,5. The non-specificity of symptoms and signs may contribute to a delay in diagnosis, often up to three years.
Pathology
Chronic thromboembolic pulmonary hypertension is characterized by organized tissue and the presence of a variable small vessel arteriopathy leading to an increased pulmonary vascular resistance and finally resulting in progressive right heart failure.
Radiographic features
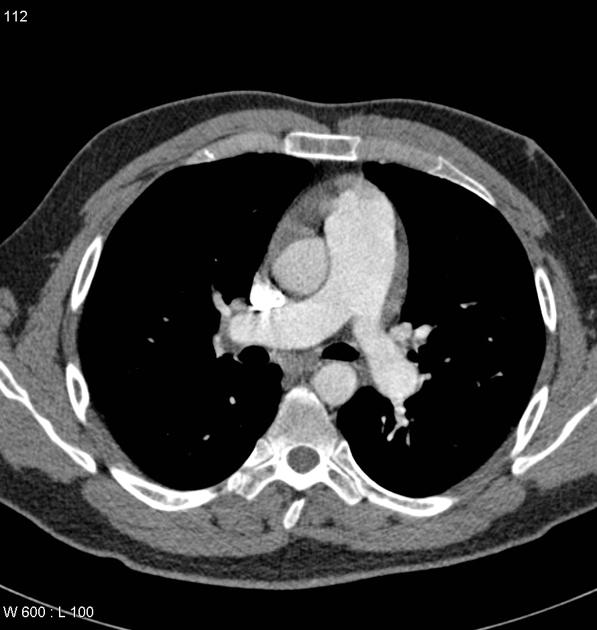
CT
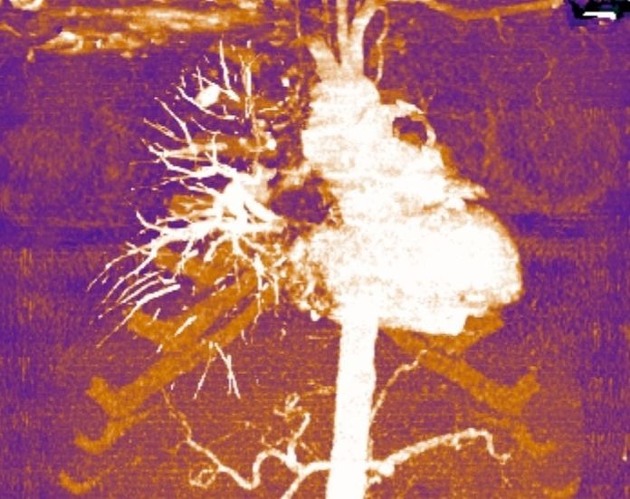
Signs of chronic thromboembolic pulmonary hypertension can be identified on unenhanced CT, contrast-enhanced CT (CE-CT) and CT pulmonary angiography (CTPA).
Pulmonary arteries
-
dilatation of the central/proximal pulmonary arteries (pulmonary artery diameter: ≥29 mm in men and ≥27 mm in women)
visible on unenhanced CT, CE-CT and CTPA
-
eccentric organized thrombi: eccentric intraluminal filling defects adherent to the pulmonary arterial wall
visible in CE-CT and CTPA
compare with the central intraluminal filling defects in acute PE, the so-called polo mint sign (dark thrombus in the center of a pulmonary artery, surrounded by the contrast medium in white)
-
total occlusions (pouch defects), or partial occlusions
visible in CE-CT and CTPA
-
stenoses, indicated by variability in the size of lobar and segmental level vessels, and/or irregular vessel caliber
visible in CTPA
-
intraluminal fibrous webs or bands, these appear as linear intraluminal filling defects; intraluminal fibrous bands are ribbon-like structures anchored to the vessel wall at two points with a free mid-portion (often oriented along the long axis of vessel) while intraluminal fibrous webs are branching networks of bands
visible in CTPA
Pulmonary veins
-
abnormal pulmonary venous filling / pulmonary vein sign 8
seen as hypodense filling defects within the pulmonary veins
Heart
-
enlargement of the right ventricle
visible on unenhanced CT, CE-CT and CTPA
-
thickening of the right ventricular wall
visible on unenhanced CT, CE-CT and CTPA
Lung
-
mosaic perfusion pattern of the lung parenchyma
visible in unenhanced CT and CE-CT
-
residual scars from infarcts (peripheral irregular, linear, or wedge-shaped densities)
visible in unenhanced CT, CE-CT and CTPA
-
large bronchial artery collaterals
visible in CE-CT
acute pulmonary embolism can also cause this appearance
Classification
Surgical resectability can be classified according to the University of California, San Diego (UCSD)-CTEPH surgical classification, and is a useful clinical addition to a report impression 9.
Treatment and prognosis
Pulmonary thromboendarterectomy (PTE) remains the guideline-recommended treatment for operable CTEPH. Other available treatments include targeted medical therapy and balloon pulmonary angioplasty 6,7.







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.