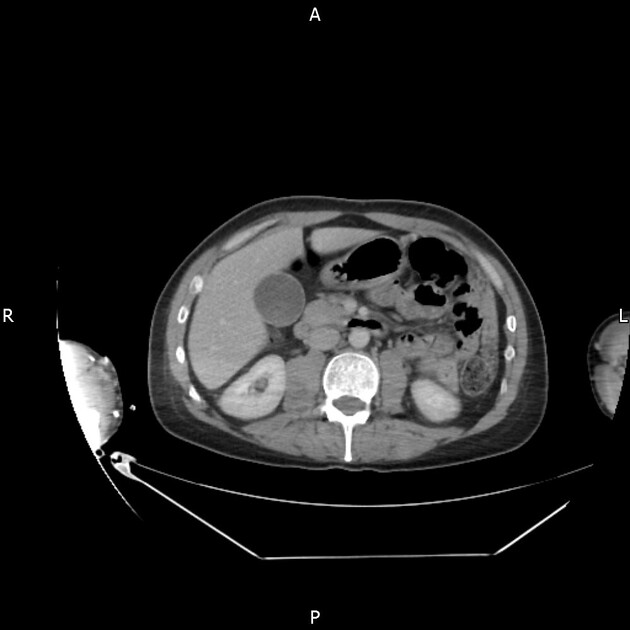
The CT neck chest-abdomen-pelvis protocol aims to evaluate the neck, thoracic and abdominal structures using contrast in trauma imaging. The use of contrast facilitates the assessment of pathologies globally whilst minimising dose by potentially disregarding a non-contrast scan.
Note: This article is a general guideline for CT imaging of the neck, chest, abdomen-pelvis. Protocol factors are variable as they depend on the CT scanner, software, patient demographics, and the radiologist.
Trauma imaging aims to evaluate multiple pathologies with a minimal radiation dose, therefore please refer to organ-specific protocols for further evaluation of structures and pathologies.
A standard CT neck, chest, abdomen, and pelvis protocol might follow as such:
Indications
Indications involve the assessment and monitoring of the following pathologies 1-3.
neck mass or adenopathy
airway compromise
oesophageal compromise
infections and inflammatory conditions
traumatic injuries, including blunt and penetrating injuries (foreign bodies)
diagnosis or evaluation of malignancies
sepsis or fever with an unknown cause
post-operative follow-up
Purpose
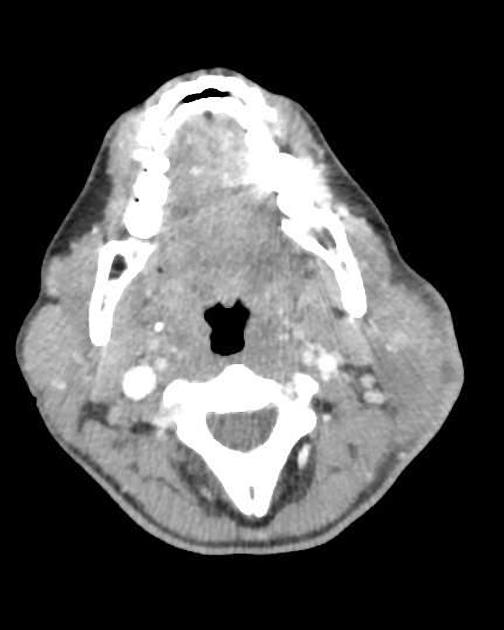
The purpose of a CT neck in conjunction with a chest abdomen-pelvis protocol (CT CAP) is to assess symptoms of inflammation, blunt or penetrating trauma, acute infection, masses, malignancies, base of skull, laryngotracheal and oesophageal injuries 1-3. CT neck can be scanned as a non-contrast, a neck angiogram or more commonly as a biphasic soft tissue neck depending on the structures being evaluated 1. A soft tissue neck focuses on the cutaneous and subcutaneous soft tissues, salivary glands, aerodigestive tract, teeth and peri-odontal tissues and lymph nodes, whilst the angiogram demonstrates cerebral arteries in greater detail 1.
A CT chest abdomen-pelvis aims to evaluate and characterise injuries resulting from trauma. The use of contrast better demonstrates the following 2:
blunt or penetrating trauma and its involvement with vasculatures
cancerous lesions/masses
vasculatures in the circumstance of haemorrhage or soft tissue oedema
gastrointestinal tract, lungs, abdomen
Technique
-
patient position
supine position, body centred within the gantry
arms up: CT chest abdomen-pelvis
arms down: CT neck
-
tube voltage
≤120 kVp
-
tube current
as per automatic exposure control (AEC)
-
scout
above lung apices to the symphysis: CT chest abdomen-pelvis
above orbits to aortic arch: CT neck
-
scan extent
above lung apices to the symphysis
above orbits to aortic arch
-
scan direction
craniocaudal for the chest abdomen-pelvis
caudocranial for the neck
-
scan geometry
field of view (FOV ): 350 mm (chest abdomen-pelvis); 140-200mm (neck)
slice thickness: (chest abdomen-pelvis): ≤0.75 mm, interval: ≤0.5 mm; (neck) ≤0.75 mm, interval: ≤0.5 mm
reconstruction algorithm: soft tissue, bone
-
oral contrast
to be administered on the table prior to scanning
contrast injection considerations
non-contrast (if contrast medium is a contraindication or not required)
-
biphasic arterial + venous acquisition + post-contrast neck
contrast volume: 70-100 mL (0.1 mL/kg) with 30-40 mL saline bolus at 3-5 mL/s
-
portal venous acquisition
60-80 seconds post contrast injection or 35-40 seconds post completion of arterial phase
-
biphasic contrast neck acquisition
-
initial bolus of contrast administered will be seen as a venous flow on the scan
an additional 40 mL of contrast is administered at 2 mL/s for 20 sec following 10 second delay before imaging
-
-
neck angiography (an alternative option to a CT soft tissue neck)
the initial bolus of contrast from the CT chest abdomen-pelvis will be visualised as venous flow depending on the patient's demographics
a second injection of 50-70 mL of contrast is administered at 4 mL/s with a 40 mL saline bolus at 4 mL/s
-
respiration phase
-
chest abdomen-pelvis
single breath hold inspiration
-
neck
do not swallow, Valsalva or puff cheeks
-
-
multiplanar reconstructions
-
chest abdomen-pelvis
sagittal images: aligned sagittal to the body axis
coronal images: aligned coronal to the body axis
axial images: aligned axial to the body axis
slice thickness: soft tissue ≤3 mm, bone ≤2 mm overlap 20-40%, lung (chest) ≤3 mm
-
neck
sagittal images: aligned to the cervical vertebral body
coronal images: aligned to the transverse process and mandible
axial images: perpendicular to the head-neck axis
slice thickness: soft tissue ≤3 mm, overlap >30%, bone ≤2 mm
-
Dynamic manoeuvres for neck imaging
The anatomical complexity of the neck makes radiological assessment difficult; hence the dual phase neck component to delineate structures, there are differing breathing instructions to aid in assessment 6
-
puffed cheeks
creates a negative contrast within the oral vestibule and helps improve the definition of mucosa, buccinator, pterygomandibular raphe, and retromolar trigone
-
valsalva manoeuvre
distends the airway and helps with the visualisation of the paraglottic fat planes
Practical points
patient positioning in correlation to the iso-centre will facilitate dose modulation depending on the region of interest, thus affecting patient position (arms up for CT chest abdomen-pelvis & arms down for CT neck)
the first contrast bolus will be visualised as the venous phase on the neck acquisition and the second contrast bolus will demonstrate the arterial phase of the neck, thus a biphasic scan 1
an angiogram can also be achieved by increasing the volume of the second contrast bolus and adjusting the trigger of the scan 1
the use of IV contrast visualises soft tissue structures, vessels and potential contrast extravasations demonstrating an active haemorrhage 3
use of oral contrast is not typical, however necessary in the circumstances of excluding oesophageal injuries 4
-
dose optimisation techniques
two scouts for dose modulation: one for the CT chest abdomen-pelvis component and one for the CT neck as patient position varies





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.