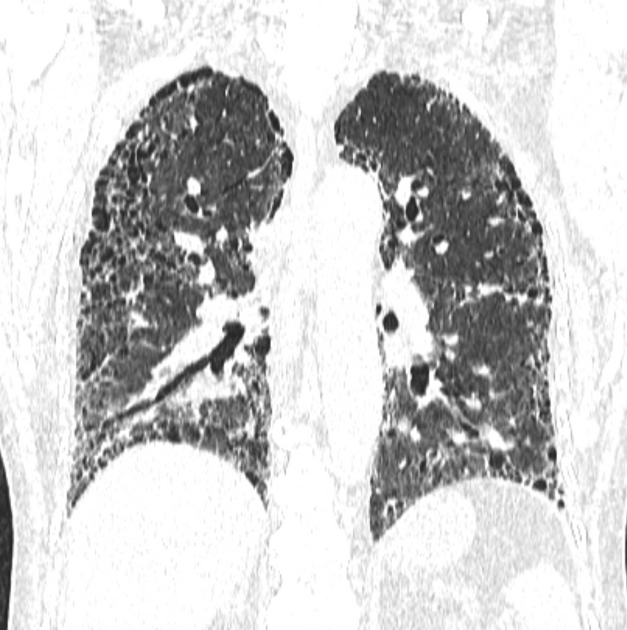
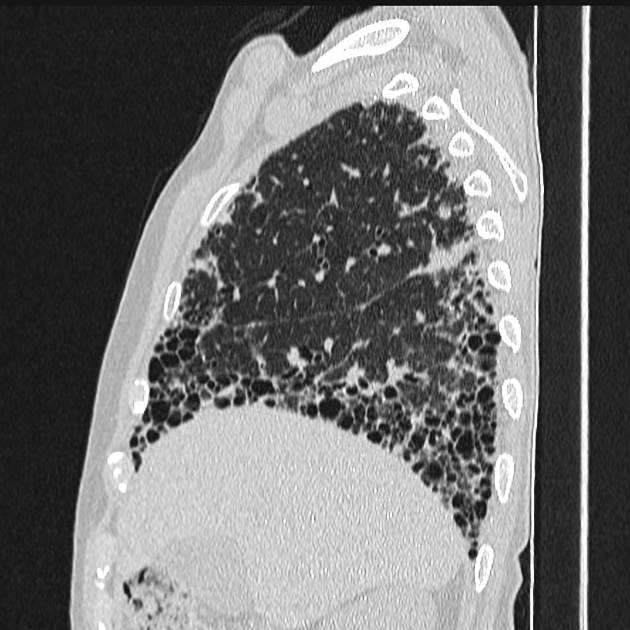
Diagnostic HRCT criteria for usual interstitial pneumonia (UIP) pattern - ATS/ERS/JRS/ALAT (2018)
Updates to Article Attributes
As a part of international evidence based guidelines adopted by collaborative effort of American Thoracic Society, the European Respiratory Society, the Japanese Respiratory Society and the Latin American Thoracic association, specific diagnostic HRCT criteria for usual interstitial pneumonia (UIP) pattern were adopted in 2011. At the time of writing (mid 2016), this is the most widely accepted classification system.
Classification
- UIP pattern (definite)
- possible UIP pattern
- inconsistent UIP pattern
This helps radiologists to determine the certainty of UIP diagnosis based on HRCT chest findings. The importance of this guideline is that definite UIP pattern on chest HRCT precludes the need for tissue diagnosis 1,2. However, unfortunately up to 20% of inconsistent with UIP group (or actually atypical UIP) can be UIP on biopsy or idiopathic pulmonary fibrosis (IPF) in clinical course.
UIP pattern
All four features present:
- subpleural, basal predominance
- reticular abnormality
- honeycombing +/- traction bronchiectasis
- absence of features listed as "inconsistent with UIP pattern"(see below)
Possible UIP pattern
All three features present:
- subpleural, basal predominance
- reticular abnormality
- absence of features listed as "inconsistent with UIP pattern" (see below)
Inconsistent with UIP pattern
Any one of the following seven features present:
- upper or mid-lung predominance
- peribronchovascular predominance
- extensive ground glass abnormality (i.e. more than reticular abnormality)
- profuse micronodules (bilateral, predominantly upper lobes)
- discrete cysts (multiple, bilateral, away from honeycombing)
- diffuse mosaic attenuation / air-trapping (bilateral in ≥3 lobes)
- consolidation in bronchopulmonary segment(s) or lobe(s)





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.