Dynamic susceptibility contrast (DSC) MR perfusion
Citation, DOI, disclosures and article data
At the time the article was created Frank Gaillard had no recorded disclosures.
View Frank Gaillard's current disclosuresAt the time the article was last revised Giorgio Maria Agazzi had no financial relationships to ineligible companies to disclose.
View Giorgio Maria Agazzi's current disclosures- Dynamic susceptibility contrast-enhanced MR perfusion
- DSC perfusion
- DSC MR perfusion
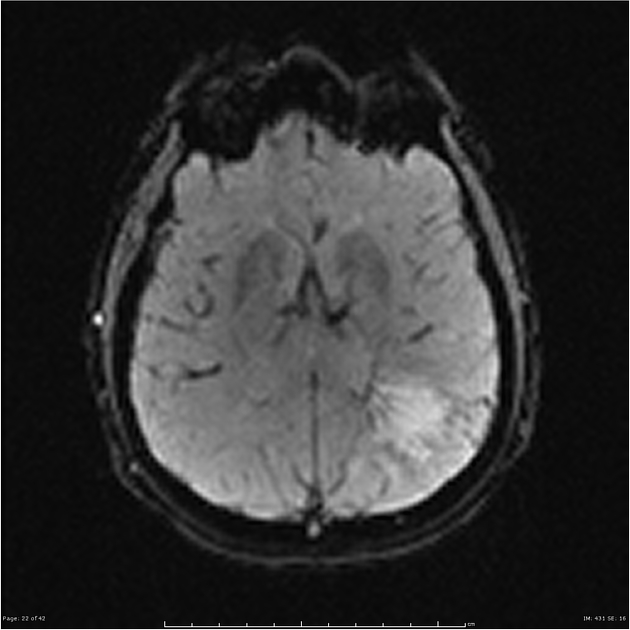
Dynamic susceptibility contrast (DSC) MR perfusion is one of the most frequently used techniques for MRI perfusion, and relies on the susceptibility induced signal loss on T2*-weighted sequences which results from a bolus of gadolinium-based contrast passing through a capillary bed. The most commonly calculated parameters are rCBV, rCBF, and MTT.
This technique is sometimes referred to, perhaps more accurately, as dynamic susceptibility contrast-enhanced MR perfusion, still abbreviated to DSC. This should not be confused with dynamic contrast-enhanced (DCE) MR perfusion, which relies on T1 shortening due to gadolinium-based contrast.
Physics and technique
DSC perfusion exploits the regional susceptibility-induced signal loss caused by paramagnetic contrast agents (such as commonly used gadolinium-based compounds) on T2-weighted images 1,2. Although this technique can be performed with both T2 (e.g. spin echo) and T2* (e.g. gradient-echo echo-planar) sequences, the former requires higher doses of contrast, which is why T2* techniques are more commonly employed 2.
A bolus of gadolinium-containing contrast is injected intravenously and rapid repeated imaging of the tissue (most commonly brain) is performed during the first pass. This leads to a series of images with the signal in each voxel representing intrinsic tissue T2/T2* signal attenuated by susceptibility-induced signal loss proportional to the amount of contrast primarily in the microvasculature 1,2.
After image acquisition, a region's signal is interrogated over the time-course of the perfusion sequence, generating a signal intensity-time curve, from which various parameters can be calculated (e.g. rCBV, rCBF, MTT). These values can then be used to create color maps of regional perfusion.
Pitfalls
Because this technique relies upon detecting signal loss due to small amounts of contrast, if there is significant signal loss due to the presence of calcification or blood products, or due to artifact from adjacent dense bone or aerated sinuses, obtained values will not be reliable. Similarly, values in a region immediately adjacent to large vessels will also be affected.
Post-processing software can also introduce difference in results, with data showing that the same DSC data analyzed with different software packages can lead to different perfusion values4.
References
- 1. Essig M, Shiroishi MS, Nguyen TB et-al. Perfusion MRI: the five most frequently asked technical questions. AJR Am J Roentgenol. 2013;200 (1): 24-34. doi:10.2214/AJR.12.9543 - Free text at pubmed - Pubmed citation
- 2. Petrella JR, Provenzale JM. MR perfusion imaging of the brain: techniques and applications. AJR Am J Roentgenol. 2000;175 (1): 207-19. doi:10.2214/ajr.175.1.1750207 - Pubmed citation
- 3. Clinical MR Neuroimaging. Cambridge University Press. (2009) ISBN:0521515637. Read it at Google Books - Find it at Amazon
- 4. Boxerman J, Quarles C, Hu L et al. Consensus Recommendations for a Dynamic Susceptibility Contrast MRI Protocol for Use in High-Grade Gliomas. Neuro Oncol. 2020;22(9):1262-75. doi:10.1093/neuonc/noaa141 - Pubmed
Incoming Links
Related articles: Imaging technology
- imaging technology
- imaging physics
- imaging in practice
-
x-rays
- x-ray physics
- x-ray in practice
- x-ray production
- x-ray tube
- filters
- automatic exposure control (AEC)
- beam collimators
- grids
- air gap technique
- cassette
- intensifying screen
- x-ray film
- image intensifier
- digital radiography
- digital image
- mammography
- x-ray artifacts
- radiation units
- radiation safety
- radiation detectors
- fluoroscopy
-
computed tomography (CT)
- CT physics
- CT in practice
- CT technology
- CT image reconstruction
- CT image quality
- CT dose
-
CT contrast media
-
iodinated contrast media
- agents
- water soluble
- water insoluble
- vicarious contrast material excretion
- iodinated contrast media adverse reactions
- agents
- non-iodinated contrast media
-
iodinated contrast media
-
CT artifacts
- patient-based artifacts
- physics-based artifacts
- hardware-based artifacts
- ring artifact
- tube arcing
- out of field artifact
- air bubble artifact
- helical and multichannel artifacts
- CT safety
- history of CT
-
MRI
- MRI physics
- MRI in practice
- MRI hardware
- signal processing
-
MRI pulse sequences (basics | abbreviations | parameters)
- T1 weighted image
- T2 weighted image
- proton density weighted image
- chemical exchange saturation transfer
- CSF flow studies
- diffusion weighted imaging (DWI)
- echo-planar pulse sequences
- fat-suppressed imaging sequences
- gradient echo sequences
- inversion recovery sequences
- metal artifact reduction sequence (MARS)
-
perfusion-weighted imaging
- techniques
- derived values
- saturation recovery sequences
- spin echo sequences
- spiral pulse sequences
- susceptibility-weighted imaging (SWI)
- T1 rho
- MR angiography (and venography)
-
MR spectroscopy (MRS)
- 2-hydroxyglutarate peak: resonates at 2.25 ppm
- alanine peak: resonates at 1.48 ppm
- choline peak: resonates at 3.2 ppm
- citrate peak: resonates at 2.6 ppm
- creatine peak: resonates at 3.0 ppm
- functional MRI (fMRI)
- gamma-aminobutyric acid (GABA) peak: resonates at 2.2-2.4 ppm
- glutamine-glutamate peak: resonates at 2.2-2.4 ppm
- Hunter's angle
- lactate peak: resonates at 1.3 ppm
- lipids peak: resonates at 1.3 ppm
- myoinositol peak: resonates at 3.5 ppm
- MR fingerprinting
- N-acetylaspartate (NAA) peak: resonates at 2.0 ppm
- propylene glycol peak: resonates at 1.13 ppm
-
MRI artifacts
- MRI hardware and room shielding
- MRI software
- patient and physiologic motion
- tissue heterogeneity and foreign bodies
- Fourier transform and Nyquist sampling theorem
- MRI contrast agents
- MRI safety
-
ultrasound
- ultrasound physics
-
transducers
- linear array
- convex array
- phased array
- frame averaging (frame persistence)
- ultrasound image resolution
- imaging modes and display
- pulse-echo imaging
- real-time imaging
-
Doppler imaging
- Doppler effect
- color Doppler
- power Doppler
- B flow
- color box
- Doppler angle
- pulse repetition frequency and scale
- wall filter
- color write priority
- packet size (dwell time)
- peak systolic velocity
- end-diastolic velocity
- resistive index
- pulsatility index
- Reynolds number
- panoramic imaging
- compound imaging
- harmonic imaging
- elastography
- scanning modes
- 2D ultrasound
- 3D ultrasound
- 4D ultrasound
- M-mode
-
ultrasound artifacts
- acoustic shadowing
- acoustic enhancement
- beam width artifact
- reverberation artifact
- ring down artifact
- mirror image artifact
- side lobe artifact
- speckle artifact
- speed displacement artifact
- refraction artifact
- multipath artifact
- anisotropy
- electrical interference artifact
- hardware-related artifacts
- Doppler artifacts
- aliasing
- tissue vibration
- spectral broadening
- blooming
- motion (flash) artifact
- twinkling artifact
- acoustic streaming
- biological effects of ultrasound
- history of ultrasound
-
nuclear medicine
- nuclear medicine physics
- detectors
- tissue to background ratio
-
radiopharmaceuticals
- fundamentals of radiopharmaceuticals
- radiopharmaceutical labeling
- radiopharmaceutical production
- nuclear reactor produced radionuclides
- cyclotron produced radionuclides
- radiation detection
- dosimetry
- specific agents
- carbon-11
- chromium-51
- fluorine agents
- gallium agents
- Ga-67 citrate
- Ga-68
- iodine agents
-
I-123
- I-123 iodide
- I-123 ioflupane (DaTSCAN)
- I-123 ortho-iodohippurate
- I-131
-
MIBG scans
- I-123 MIBG
- I-131 MIBG
-
I-123
- indium agents
- In-111 Octreoscan
- In-111 OncoScint
- In-111 Prostascint
- In-111 oxine labeled WBC
- krypton-81m
- nitrogen-13
- oxygen-15
- phosphorus-32
- selenium-75
-
technetium agents
- Tc-99m DMSA
- Tc-99m DTPA
- Tc-99m DTPA aerosol
- Tc-99m HMPAO
- Tc-99m HMPAO labeled WBC
- Tc-99m MAA
- Tc-99m MAG3
- Tc-99m MDP
- Tc-99m mercaptoacetyltriglycine
- Tc-99m pertechnetate
- Tc-99m labeled RBC
- Tc-99m sestamibi
- Tc-99m sulfur colloid
- Tc-99m sulfur colloid (oral)
- thallium-201 chloride
- xenon agents
- in vivo therapeutic agents
- pharmaceuticals used in nuclear medicine
-
emerging methods in medical imaging
- radiography
- phase-contrast imaging
- CT
- deep-learning reconstruction
- photon counting CT
- virtual non-contrast imaging
- ultrasound
- magnetomotive ultrasound (MMUS)
- superb microvascular imaging
- ultrafast Doppler imaging
- ultrasound localization microscopy
- MRI
- nuclear medicine
- total body PET system
- immuno-PET
- miscellaneous
- radiography





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.