The clinical history will nearly always lead to a short differential or the answer. Show off to the examiner that you have a structured approach to reporting and managing the patient.
Structured approach
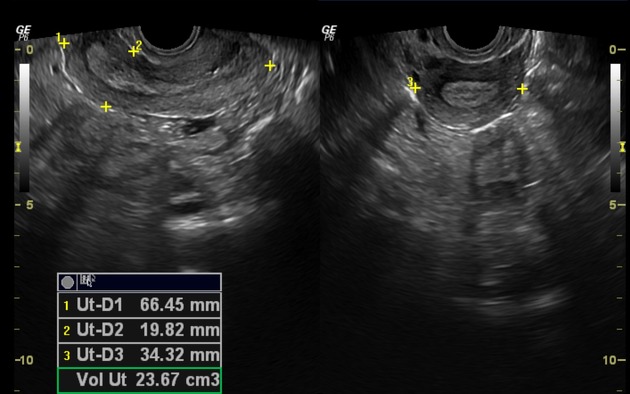
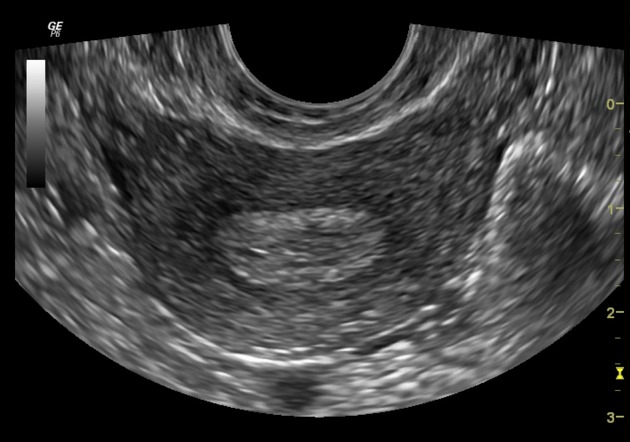
- uterus: size, version and shape (normal or variant which you should elaborate on and say what it most likely is e.g. arcuate, septate, bicornuate and state that you would always perform a 3D ultrasound to evaluate it)
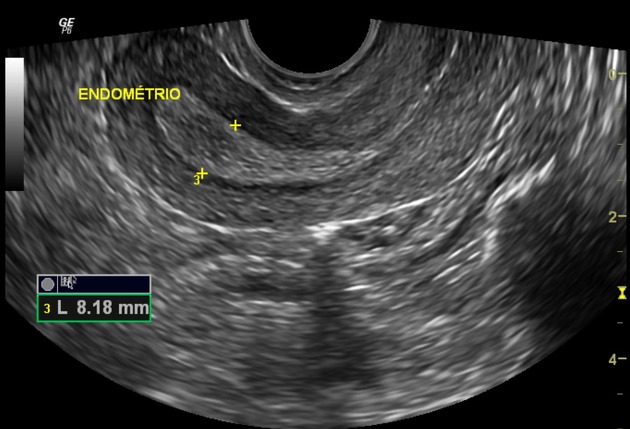
- endometrium: thickness and phase in the menstrual cycle (thin with oral contraceptive pill (OCP))
- myometrium: normal, focal thickness or abnormality, generalized thickness
- serosa: normal or fibroid
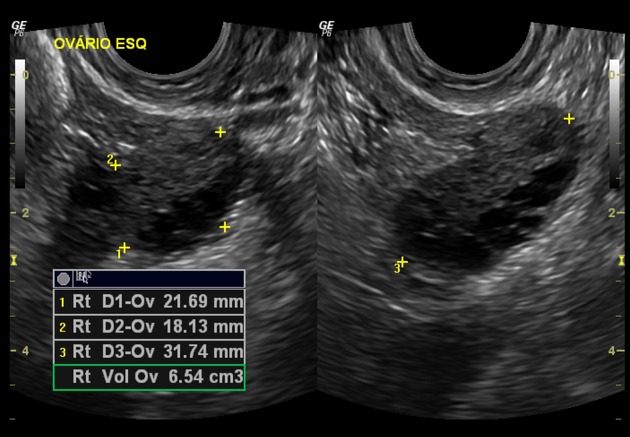
- ovaries: normal, cystic or mass
- pelvic fluid: not present, small or large volume, sonolucent or echogenic
Normal example: transabdominal and transvaginal pelvic images demonstrate a normal uterus that is anteverted/retroverted and measures 80 x 35 x 50 mm. The endometrium has a normal thickness of 3 mm, normal vascularity, and is in the menstrual/proliferative or secretory phase. The myometrium and serosa have a normal appearance. Both ovaries have a normal size and appearance, and there is a trace of fluid in the pouch of Douglas.
Clinical history
-
per vaginal bleeding
- premenopausal
- pregnancy related
- postmenopausal
- pelvic pain
- infertility/subfertility
- hyperandrogenism





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.