Intracranial atherosclerotic disease (ICAD), also known as intracranial atherosclerosis or intracranial atherosclerotic stenosis (ICAS), is the term applied to atherosclerosis of the large intracranial arteries and is a cause of recurrent ischemic stroke.
On this page:
Epidemiology
Intracranial atherosclerotic disease is an important cause of ischemic stroke in certain racial groups, particularly Asians, but also Hispanics and Black populations 7. Intracranial atherosclerotic disease is identified in up to ~50% of Asian patients with ischemic stroke 1,6,7. In White populations, however, intracranial atherosclerotic disease is an uncommon cause (approximately ~10%) of ischemic stroke 5,7.
Risk factors
The traditional risk factors for atherosclerosis apply to intracranial atherosclerotic disease, particularly 4:
Clinical presentation
Asymptomatic intracranial atherosclerotic disease is commonly diagnosed incidentally in brain imaging given the abundance of neuroimaging performed worldwide. When symptomatic, intracranial atherosclerotic disease can present as either:
progressive chronic white matter ischemia, which can lead to cognitive impairment
convexal subarachnoid hemorrhage (rare), due to rupture of compensatory dilated pial vessels 10
Pathology
The most common locations for intracranial atherosclerotic disease include arteries that have a diameter >3 mm, including 4:
-
typically in the proximal M1 segment
may be present in up to 30% of asymptomatic Asian patients with relevant vascular risk factors 6
basilar artery: typically in the distal segment
intracranial internal carotid artery
Intracranial atherosclerotic disease can cause ischemic stroke through a number of mechanisms 4,6,7:
artery-to-artery embolism, causing distal branch ischemic stroke
atherosclerosis encroaching the ostia of perforators, causing lacunar ischemic stroke
hypoperfusion, causing border zone ischemic stroke (considered rare)
thrombotic occlusion at site of intracranial atherosclerotic disease, causing large vessel occlusive ischemic stroke (considered rare)
For pathogenesis of the processes leading to intracranial atherosclerotic disease, see the atherosclerosis article.
Radiographic features
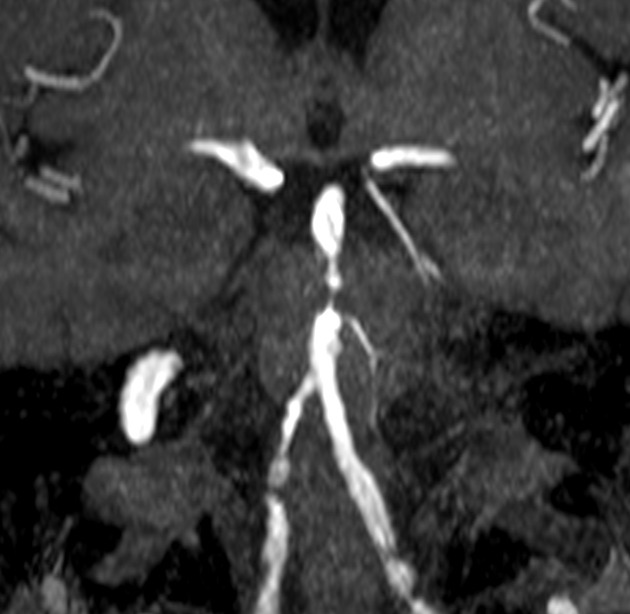
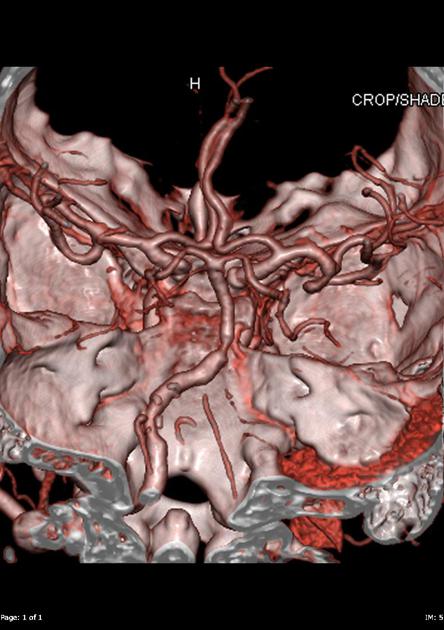
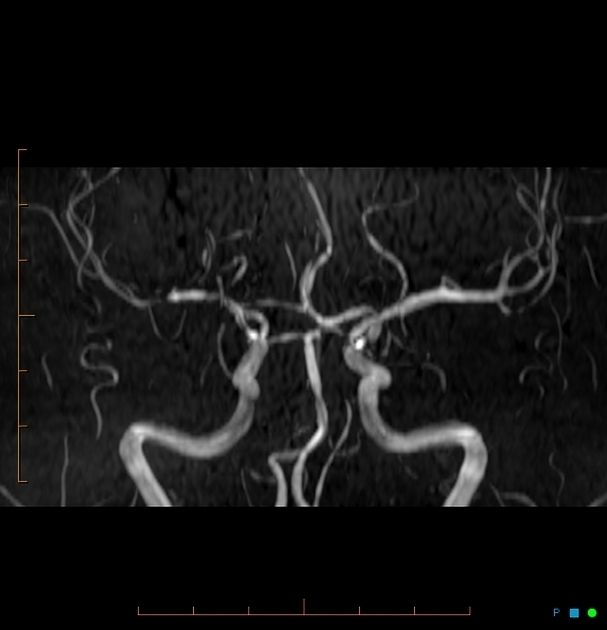
CT angiography, MR angiography, angiography (DSA), and ultrasound are the main modalities which identify focal eccentric arterial stenoses and occlusion seen in intracranial atherosclerotic disease 4. Significant stenosis is variably defined by stenosis of ≥50-70% 7.
Ultrasound
Transcranial Doppler (TCD) ultrasound can be used to obtain hemodynamic and luminal information reliably in intracranial atherosclerotic disease of 50-99% 7, but is highly operator-dependent and requires adequate bone windows 4. In regions of intracranial atherosclerotic disease, there is 7:
increased mean flow velocity
reduced distal mean flow velocity
increased pulsatility index
Intravascular ultrasound (IVUS) can be used in conjunction with DSA to assess plaque stability and composition, similar to its more accepted use in coronary artery disease 8.
CT
CT angiography is the main modality used in the diagnosis of intracranial atherosclerotic disease 7. Compared to DSA, it is highly sensitive and specific in the diagnosis of intracranial atherosclerotic disease with stenosis >50% 7. Intracranial artery calcification may also be appreciated, however, this is not always associated with intracranial atherosclerotic disease and does not provide information regarding plaque morphology 7.
CT perfusion may show subtle abnormalities in intracranial atherosclerotic disease, including increases in mean transit time in the vascular territory distal to the region of stenosis 7. Presence of this abnormalities correlates to an increased risk of ischemic stroke 7.
Angiography (DSA)
DSA is the gold standard for assessment of hemodynamic and luminal information, however, compared to other imaging modalities, does not provide information regarding plaque morphology 4,7. The invasive nature of DSA, including the inherent ischemic stroke risk with performing the procedure, also limits its utility 7.
In patients with large vessel occlusion undergoing endovascular clot retrieval, a tapered angiographic appearance of the occlusion may be suggestive of underlying intracranial atherosclerotic disease 9.
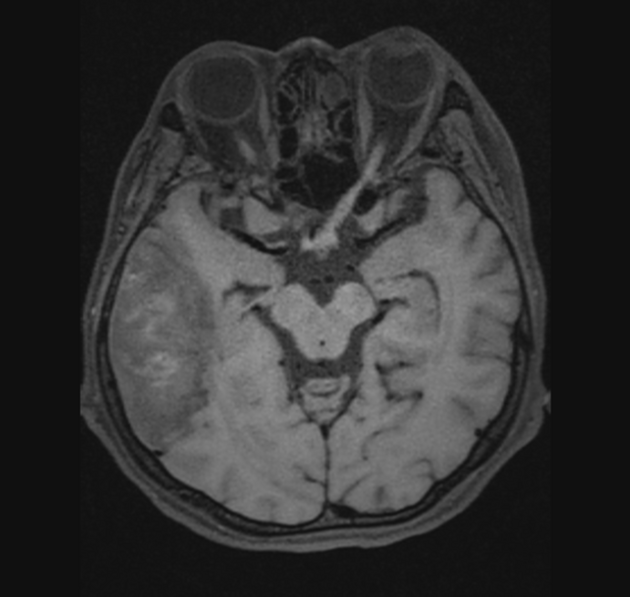
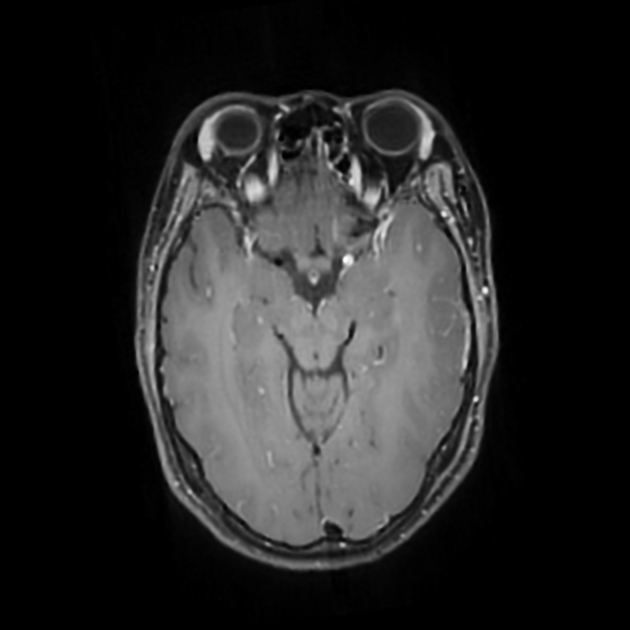
MRI
MR angiography, similar to CT angiography, is highly sensitive and specific in the diagnosis of intracranial atherosclerotic disease compared to DSA 7. Contrast-enhanced MR angiography is thought to be superior to time-of-flight MR angiography 7.
High-resolution vessel wall MRI (VW-MRI) is useful to characterize plaque morphology and differentiate plaque from other differential diagnoses (e.g. vasospasm or vasculitis), demonstrating eccentric wall thickening that is often heterogeneously enhancing 4,7. Plaque enhancement, rather than eccentric thickening, has been shown to be associated strongly with increased ischemic stroke risk 7.
Treatment and prognosis
The mainstay of acute treatment in the setting of ischemic stroke is with antiplatelet medications, often initially with dual antiplatelet therapy (e.g. for 3 months) before transition to lifelong antiplatelet monotherapy 5. Additionally, it is crucial to aggressively manage associated modifiable risk factors, such as hyperlipidemia 5,11.
Surgical treatments such as intracranial endarterectomy and extracranial to intracranial bypass procedures have been trialed, with limited evidence, but lost popularity with the emergence of endovascular techniques, such as balloon angioplasty and endovascular stenting. There are mixed randomized control trials in this space, with multiple negative or equivocal trials for endovascular stenting compared to best medical management 12-14, however, there is one positive trial for balloon angioplasty compared to best medical management 15. Generally, these endovascular techniques are considered in patients who fail best medical management 5.
The rate of ischemic stroke recurrence in patients with intracranial atherosclerotic disease may be up to ~30% within two years 7.
Differential diagnosis
intraluminal thrombus
large and medium vessel CNS vasculitis
-
intracranial arterial dissection
spontaneous
traumatic





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.