Intraductal papillary mucinous neoplasms or tumors (IPMNs or IMPTs) are epithelial cystic pancreatic tumors of mucin-producing cells that arise from the pancreatic ducts. They are most commonly seen in elderly patients. On imaging, particularly MRCP, they are characterized by single or multiple unilocular or septated pancreatic cystic lesions communicating with the pancreatic ducts.
On this page:
Epidemiology
These tumors are most frequently identified in older patients, 50-60 years of age 6, and thus are sometimes colloquially referred to as the "grandfather lesion". The main duct type appears to present around a decade earlier than branch duct type 5. The sex distribution is roughly balanced with a possible slight male predominance 15.
Clinical presentation
Clinical presentation can be difficult to distinguish from chronic pancreatitis with repeated acute exacerbations. Patients can present with abdominal pain, weight loss, obstructive jaundice, pancreatitis and new-onset diabetes mellitus 5,9.
Pathology
Intraductal papillary mucinous neoplasms are one of several mucinous tumors of the pancreas and can be further divided both histologically and with respect to their macroscopic appearance 5.
Location
Reported locations of IPMN include 15:
head ~50%
tail ~7%
uncinate process ~4%
elsewhere throughout the pancreas ~40%
Macroscopic appearance
Divided macroscopically:
-
main duct type
reminiscent of chronic pancreatitis
segmental or diffuse distribution
-
highest malignant potential 6
~60% are malignant 10
-
branch duct type
mostly seen in the head and uncinate process
more localized and mass-like
may be multifocal 13
may be macro- or microcystic in appearance 5
-
typically indolent behavior 6
~5% (range 2-10%) are malignant 11,12
-
mixed type
similar to the main duct type in terms of prognosis and overall survival
Solid components, as well as bile duct dilatation 14, are suspicious of malignant transformation.
Microscopic appearance
They are histologically divided into:
adenoma
borderline-malignant
intraductal papillary mucinous adenocarcinoma
Markers
In patients without pancreatitis, abnormal (either elevated or depressed) pancreatic enzyme markers (amylase/lipase) are associated with malignant IPMN, with the elevation of these a marker of invasiveness 8.
Radiographic features
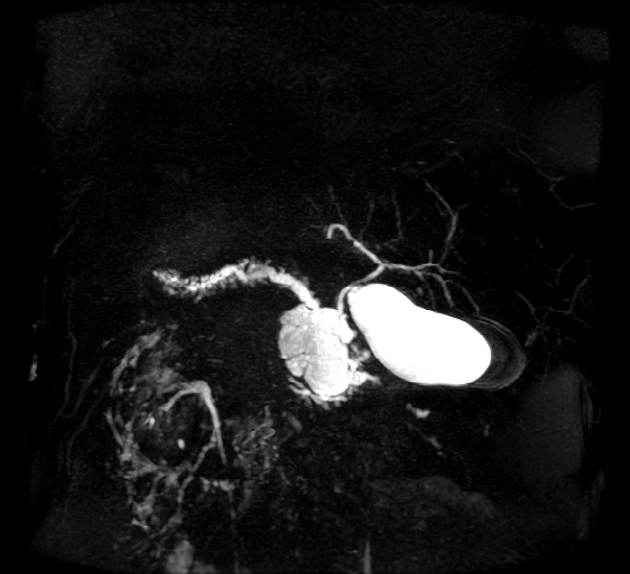
The characteristic feature is that these tumors communicate with the main pancreatic duct or its branches, which helps distinguish them from mucinous cystadenoma/cystadenocarcinoma, which do not.
Calcifications have been reported in retrospective imaging analyzes of resected IPMN at an incidence of ~13% (range 5-20%) 17-21, however, the overall incidence of calcifications in all IPMNs (i.e. resected and unresected) is not known (c.2023) and, interestingly, calcifications are not a criterion in the Kyoto guidelines to help guide whether surgical treatment is appropriate and are much more common in other pancreatic cystic lesions (e.g. serous cystadenomas).
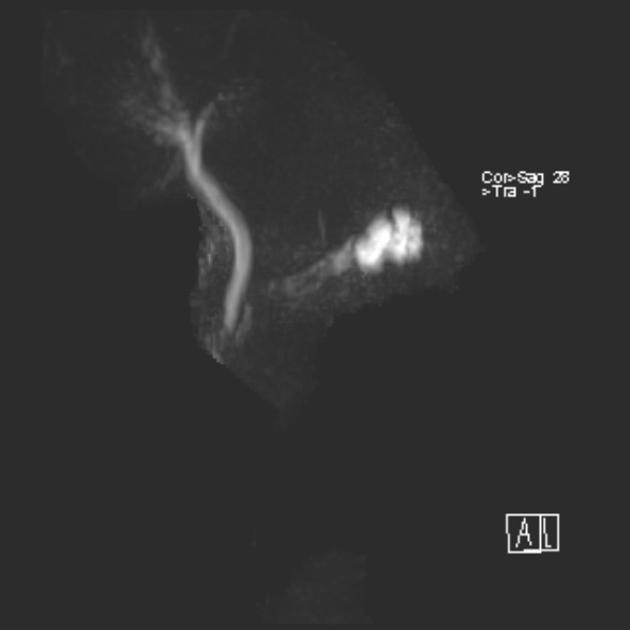
Fluoroscopy
ERCP
Direct imaging of the pancreatic duct demonstrates variable dilatation (segmental, diffuse, or branch) depending on the type. Polypoid mural tumor or amorphous mucinous luminal filling defects may be identified 5.
Mucinous material may be seen protruding from the ampulla of Vater 6.
Ultrasound
Ultrasound may demonstrate small thin-walled pancreatic cysts or dilated hypoechoic ducts (main pancreatic duct over 5 mm in caliber). Diffuse main duct type appears essentially indistinguishable from chronic pancreatitis, with duct dilatation and parenchymal atrophy 5.
Mural nodules and mucin globules may appear hyperechoic and difficult to separate from adjacent pancreatic parenchyma 6.
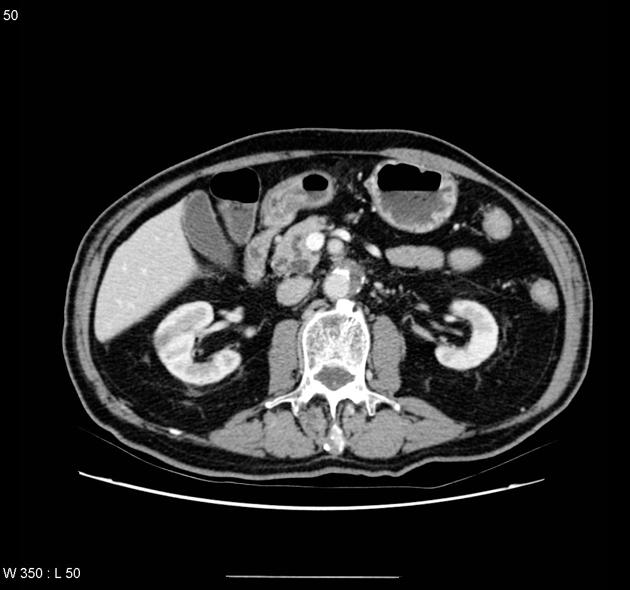
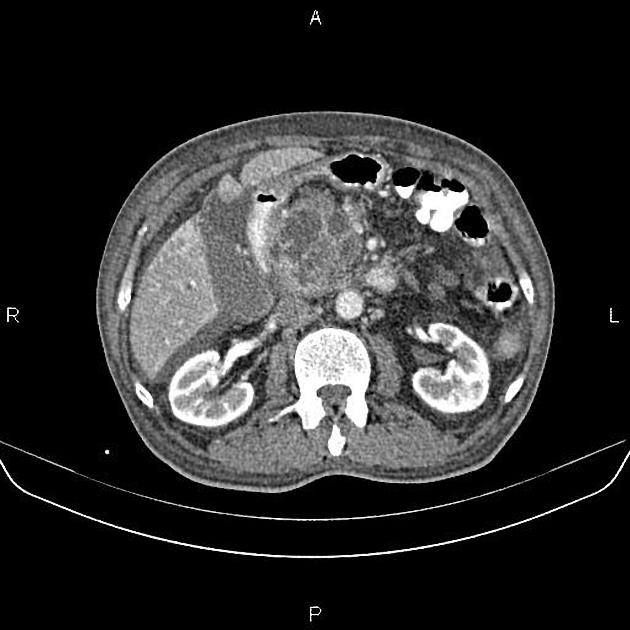
CT
They present as single or multiple pancreatic cystic hypodense lesions. Dilatation of the main duct over 5 mm concerns the main duct type IPMN. The communication with the pancreatic ducts, particularly the side branch lesions, may be difficult to demonstrate on CT. They do not calcify.
Both a dedicated pancreatic CT protocol and pancreatic MRI/MRCP have been reported as having similar accuracy in the characterization of the pancreatic cystic lesions 16, but guidelines recommend MRI as the modality of choice for IPMN follow-up.
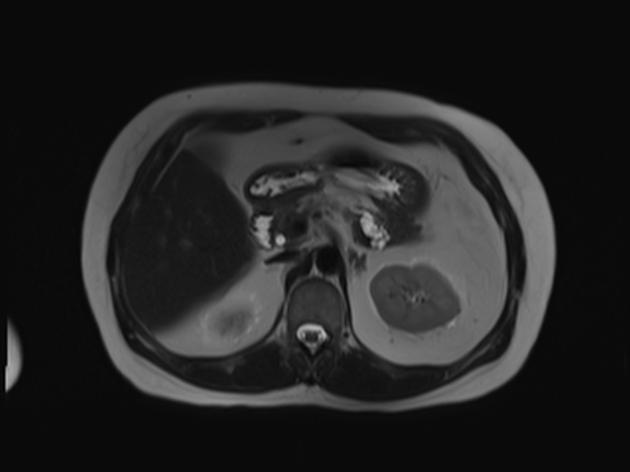
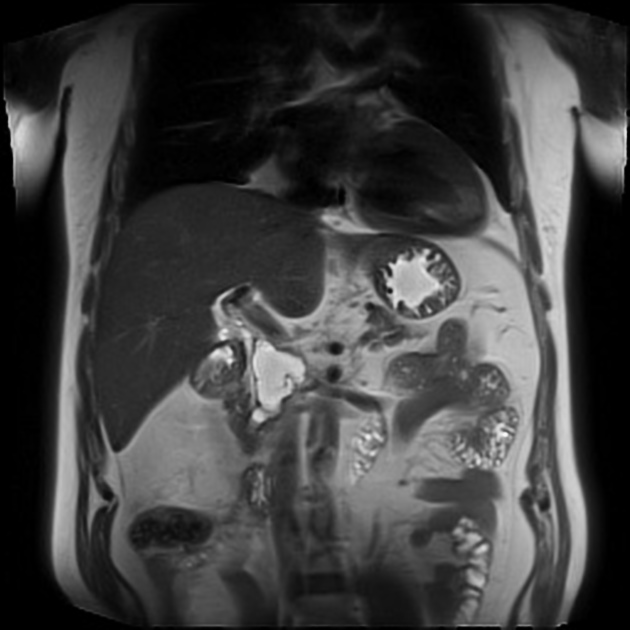
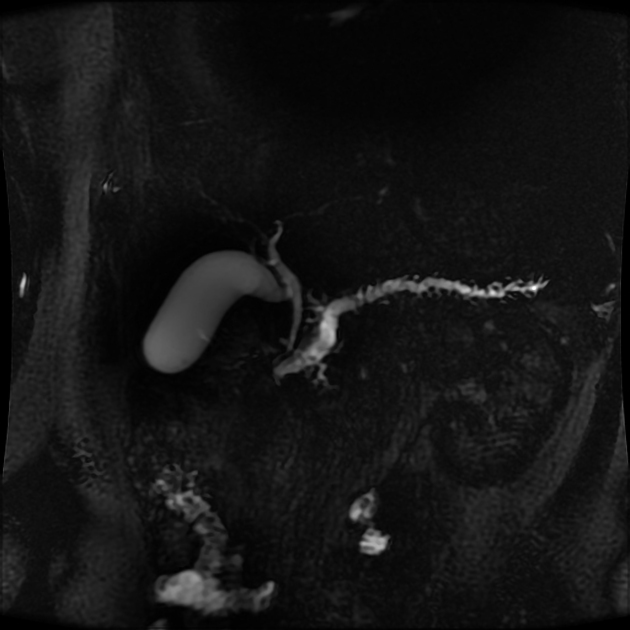
MRI
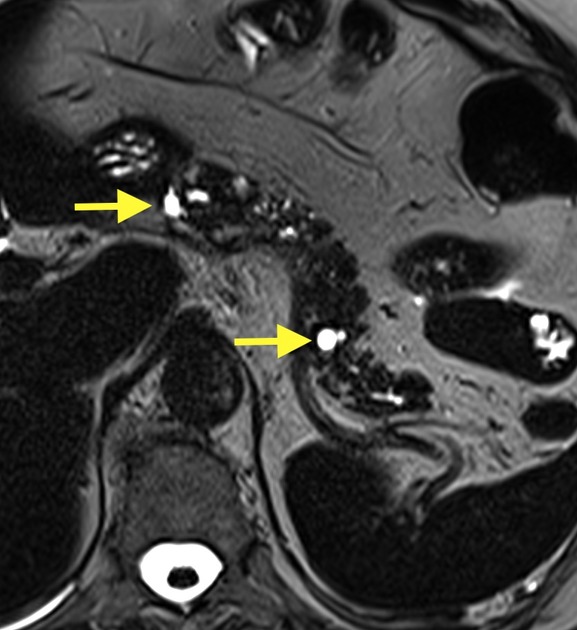
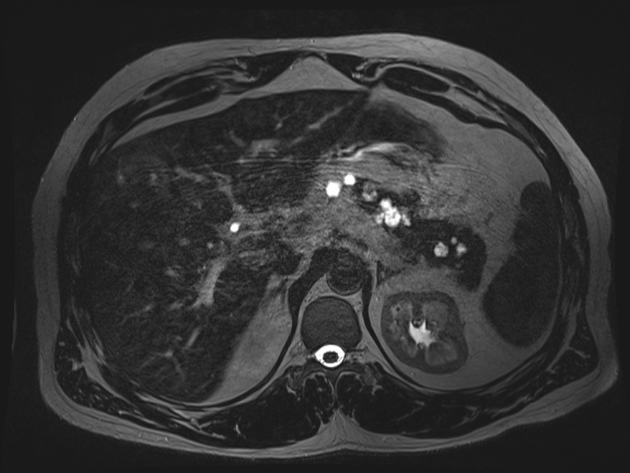
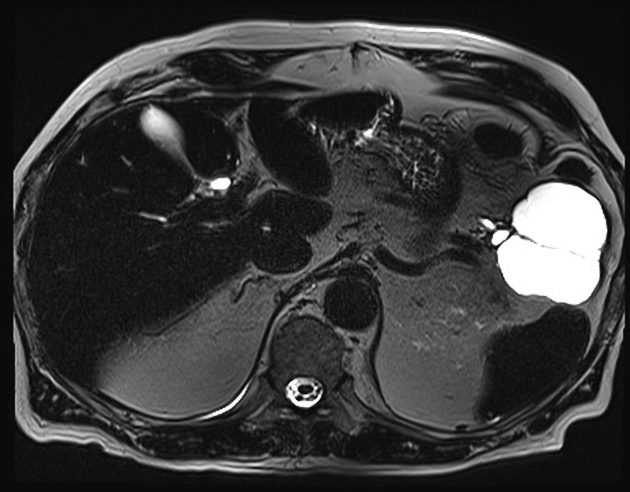
MRI, particularly MRCP, is considered the most sensitivity modality to characterize IPMNs 23.
-
main duct type
segmental or diffuse main pancreatic duct dilatation >5 mm without stricture 22,23
pancreatic parenchymal atrophy is common 23
bulging duodenal papilla: due to mucinous distension of the ampulla of Vater; a less common but highly specific (>97%) finding 22
-
solid mural nodules are concerning for malignant transformation, particularly if enhancing following administration of contrast ref
the absence of mural nodules does not exclude malignancy 22
mucin globules do not enhance and lie dependently within the duct
-
branch duct type
the majority of the gland is normal in appearance, except for a single or multifocal cystic lesions that communicate with the main pancreatic duct 23
these can measure between a few millimeters to a few centimeters 23
cystic mass-like appearance, which has been has been termed a bunch of grapes although uncommonly can be unilocular 22
-
mixed type
appears like an advanced branch duct IPMN with main pancreatic duct dilatation over 5 mm 23
See the Kyoto guidelines for further details.
Treatment and prognosis
Although generally indolent, malignant degeneration does occur, with direct invasion into adjacent organs or, more frequently, dissemination in the peritoneal cavity (pseudomyxoma peritonei).
Consensus criteria recommend resection for main duct type IPMNs and varying treatment of branch duct type IPMNs, ranging from resection to surveillance, depending on high-risk stigmata and worrisome features (see Kyoto guidelines). Patient co-morbidities and wishes clearly have a major impact on the decision to operate.
If the lesion is proximal (either segmental main duct type or branch type), a Whipple procedure may be performed. If distal, a partial pancreatectomy suffices. Complete resection is curative.
Differential diagnosis
Main duct IPMN
chronic pancreatitis: can be difficult to distinguish from main duct type on account of dilated duct 5 but main duct strictures and pancreatic stones are far more common in chronic pancreatits 22
Branch-type IPMN
mucinous cystadenoma/cystadenocarcinoma: should not appear to communicate with the main pancreatic duct 23
-
should not appear to communicate with the main pancreatic duct 23
appear similar to microcystic branch type IPMN 23
central stellate scar +/- calcification 23
-
should not appear to communicate with the main pancreatic duct 23
more commonly unilocular 22
Practical points
The radiological report has to be clear regarding imaging worrisome features of these lesions that may guide further surgical intervention:
-
main duct type
main pancreatic duct over 5 mm
presence of contrast-enhancing components
-
branch duct type
main pancreatic duct over 5 mm
cyst diameter ≥3 cm
presence of a contrast-enhancing mural nodule ≥5 mm 16
presence of solid mass 16
thickened and enhancing cyst wall
growth rate ≥5 mm/year
Clinical features to guide surgery may also include:
increased serum CA 19-9 level
-
endoscopic ultrasound (EUS) with FNA sampling
cytology: differentiate between benign and lesions with either high-grade dysplasia or cancer
KRAS/GNAS mutation analyzes 16
-
new onset of 16
















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.