Intralabyrinthine schwannomas, schwannomas that arise within the membranous labyrinth (cochlea, vestibule, or semicircular canals), are uncommon compared to vestibular schwannomas and can be challenging to diagnose.
On this page:
Terminology
It should be noted that the term intralabyrinthine schwannoma is usually reserved for tumors that are entirely confined to the labyrinth. This, therefore, does not include an extension of an intercanalicular vestibular schwannoma into the labyrinth, which is far more common.
Additionally, a number of growth patterns are recognized with specific terms to denote each one 2:
-
intravestibular: tumor within the vestibule +/- extension into semicircular canals
- transmacular: vestibular tumor with a small portion of tumor extending through the macula cribrosa into the internal acoustic meatus
-
intracochlear (intracochlear schwannoma): tumor within the turns of the cochlea
- transmodiolar: cochlear tumor with a small portion of tumor extending through the modiolus into the internal acoustic meatus
- vestibulocochlear: tumor involves both vestibule and cochlea but does not extend into the internal acoustic meatus or middle ear
- transotic: tumor that extends through the labyrinth from internal acoustic meatus to middle ear cavity
The most common type is intravestibular, and the least common types are the intravestibulocochlear and the transotic 3.
Clinical presentation
Intralabyrinthine schwannomas typically present with unilateral sensorineural hearing loss, tinnitus or vertigo 1,2.
Pathology
Intralabyrinthine schwannomas arise from the Schwann cells of the terminal branches of the vestibulocochlear nerve 1. See acoustic schwannoma article for a description of histology.
Location
Intralabyrinthine schwannomas are not evenly distributed throughout the inner ear 1,2.
- cochlear: 60-80% (intracochlear and transmodiolar)
- vestibular: 15-30% (intravestibular and transmacular)
- vestibulocochlear: 5%
- transotic: <5%
Radiographic features
CT
Identifying intralabyrinthine schwannomas on CT is difficult if not impossible unless there is substantial remodeling of the surrounding bone.
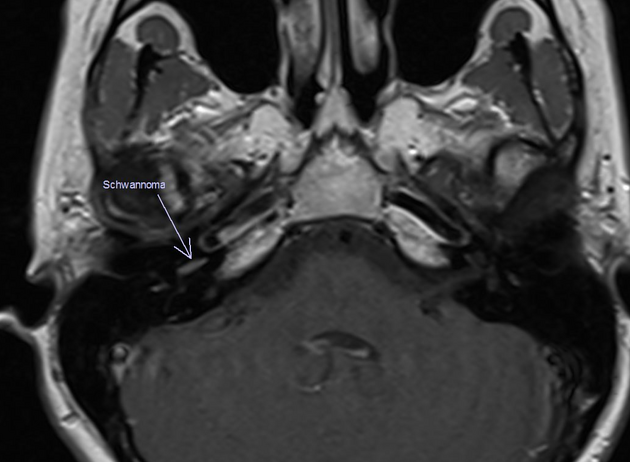
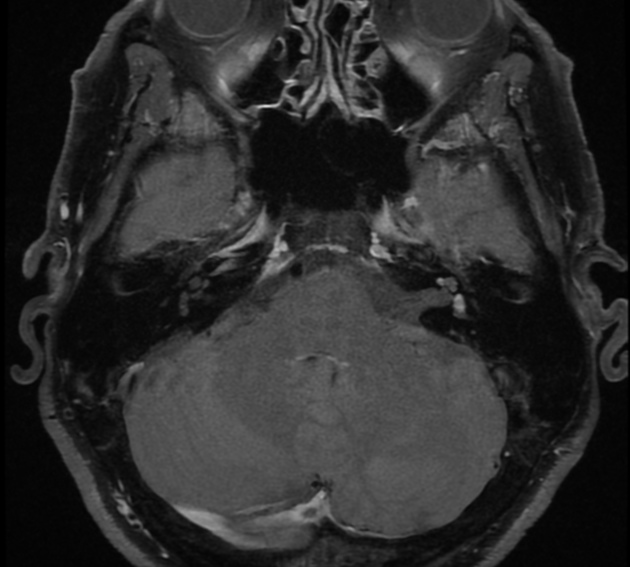
MRI
MRI is the modality of choice for assessment of potential intralabyrinthine schwannoma as it allows not only identification but also localization of the tumor within the labyrinth. Adequate assessment requires high-resolution high-contrast T2 weighted images (e.g. FIESTA or CISS).
Signal intensities are as follows 1:
- T1: slightly hyperintense to normal intralabyrinthine fluid
- T2: hypointense to normal intralabyrinthine fluid
- T1 C+: vivid enhancement
The key to diagnosis is recognizing a filling defect within the labyrinth that contrast enhances following the administration of gadolinium.
Treatment and prognosis
Although historically they have been said to usually not enlarge, some series show growth in more than 50% of cases and thus followup is required 1. Treatment is usually reserved for tumors that are growing and threatening nearby structures (e.g. facial nerve) 1.
Unlike many acoustic schwannomas where resection can be hoped to preserve hearing, operating on intralabyrinthine tumors invariably results in profound if not complete ipsilateral hearing loss 2.
Differential diagnosis
The imaging differential is primarily that of other causes of intralabyrinthine enhancement or intralabyrinthine filling defect on MR 1,2:
- acute labyrinthitis
- enhancement usually affects the entire labyrinth, is less sharply demarcated, and is more pronounced
- usually no soft tissue filling defect
-
labyrinthitis ossificans
- no enhancement
- may be diagnosed by temporal bone CT and compatible medical history (eg, remote meningitis)
- hemorrhage
- hyperintense on T1 precontrast
- intralabyrinthine lipoma
- hyperintense on T1 precontrast




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.