Intraventricular haemorrhage denotes the presence of blood within the cerebral ventricular system. It is associated with significant morbidity due to the risk of obstructive hydrocephalus.
It can be divided into primary or secondary, with primary haemorrhage being far less common than secondary:
primary: blood in the ventricles with little (if any) parenchymal blood
secondary: a large extraventricular component is present (e.g. parenchymal or subarachnoid) with secondary extension into the ventricles
In adults, secondary intraventricular haemorrhage is usually the result of an intracerebral haemorrhage (typically basal ganglia hypertensive haemorrhage) or subarachnoid haemorrhage with ventricular reflux.
Intraventricular haemorrhage is a distinct entity in paediatrics and is considered separately; see intraventricular haemorrhage of the newborn.
On this page:
Epidemiology
There are numerous causes of intraventricular haemorrhage and as such no single demographic can be identified; rather each underlying aetiology contributes its own patient population. Having said that, secondary haemorrhage is far more common and as such the dominant demographic is that of patients with intraparenchymal or subarachnoid haemorrhage: older individuals are thus most commonly affected.
Clinical presentation
Clinical presentation of intraventricular haemorrhage (regardless of cause) is similar to that of subarachnoid haemorrhage. Patients experience sudden onset of severe headache 2. Signs of meningism are also present (i.e. photophobia, nausea and vomiting and neck stiffness). Larger haemorrhages can result in loss of consciousness, seizures, and brainstem compression with cardiorespiratory compromise.
Pathology
Aetiology
Secondary intraventricular haemorrhage is much more common than primary intraventricular haemorrhage 5.
Primary
Some of the more common causes of primary intraventricular haemorrhage in adults include 2,5:
-
aneurysm (e.g. PICA aneurysms have a tendency to fill the 4th ventricle, with little basal cistern blood)
subependymal cavernous malformations
anticoagulation therapy/coagulopathy
-
adjacent parenchymal tumours (e.g. glioblastoma)
Secondary
Secondary causes of intraventricular haemorrhage include:
-
extension from other intracerebral haemorrhages
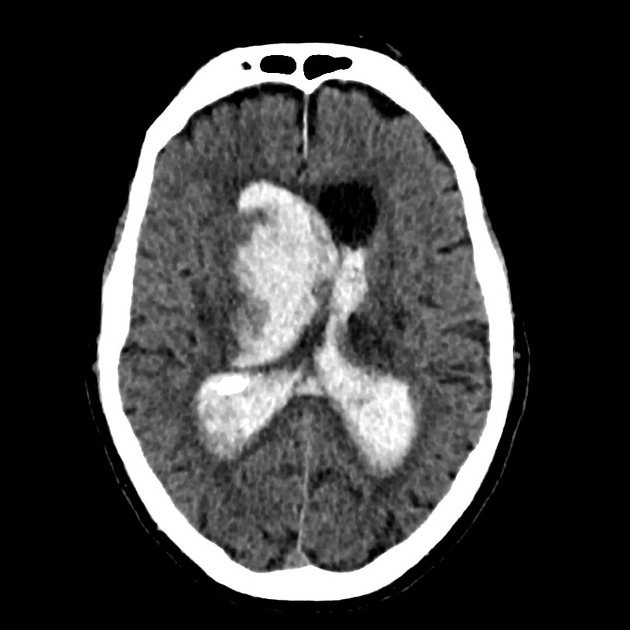
hypertensive haemorrhage, especially basal ganglia haemorrhage (common)
trauma
Radiographic features
CT
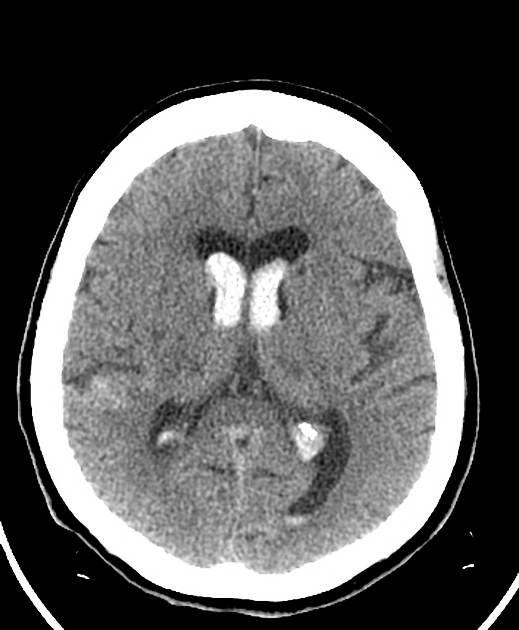
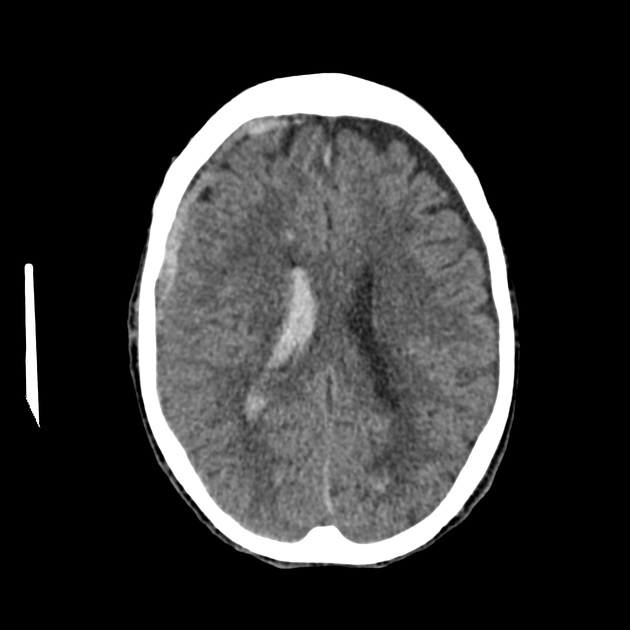
Non-contrast CT of the brain is the mainstay of acute evaluation of patients presenting with sudden onset headache or stroke-like symptoms. Blood in the ventricles appears as hyperdense material, heavier than CSF and thus tends to pool dependently, best seen in the occipital horns. Acutely, if the volume is significant, blood can fill the ventricle and clot, forming a "cast".
There is often obstructive hydrocephalus, and care must be taken in distinguishing this from ex vacuo dilatation of the ventricles.
MRI
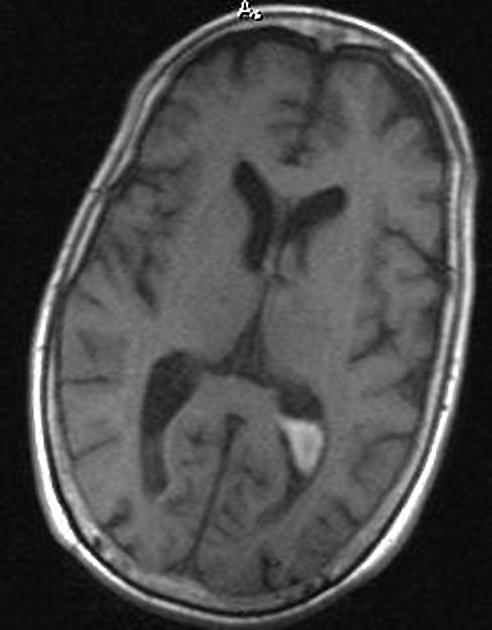
MRI is more sensitive than CT to very small amounts of blood, especially in the posterior fossa, where CT remains marred by artifact.
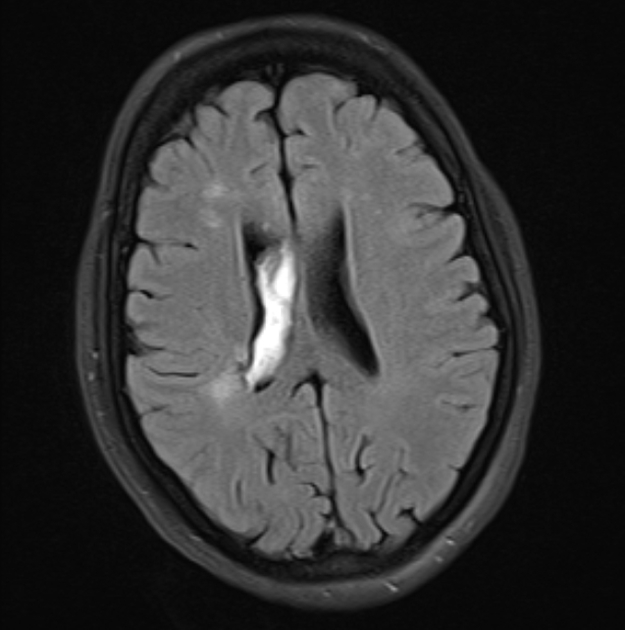
Both FLAIR and SWI (especially at 3 T) are sensitive to small amounts of blood. The latter will especially demonstrate tiny amounts of blood pooling in the occipital horns, resulting in susceptibility-induced signal dropout 3,4.
On FLAIR the signal intensity will vary depending on the timing of the scan. Within 48 hours blood will appear as hyperintense to the attenuated adjacent CSF 4. Later the signal is more variable and can be difficult to distinguish from flow-related artifact (particularly in the third and fourth ventricles) unless other sequences are also used.
Treatment and prognosis
The main treatment approaches for intraventricular haemorrhage can be divided into two:
treatment of the underlying cause of haemorrhage (e.g. aneurysm, AVM)
treatment of obstructive hydrocephalus
The latter may merely require careful monitoring of clinical state and serial CTs to assess ventricular size or may require ventricular drain placement. A number of patients will go on to require permanent CSF diversion (VP shunt).













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.