This is a basic article for medical students and other non-radiologists
Multiple sclerosis (MS) is a chronic demyelinating condition affecting the central nervous system. Diagnosis requires good history, clinical examination, appropriate imaging, and laboratory tests (cerebrospinal fluid for IgG index and oligoclonal bands).
It is typified by "plaques" of disease which are spread by location and time. MRI is frequently the first-line imaging modality for diagnosis and follow-up.
On this page:
Reference article
This is a summary article; read more in our article on multiple sclerosis.
Summary
-
epidemiology
- worldwide condition with strong geographical variation 1
- overall prevalence is 30 per 100,000
- the average of onset is 29 years
- cases recognized from teens to over-60s
- there is a strong female preponderance - M:F = 1:2-3
- worldwide condition with strong geographical variation 1
-
presentation
- depends on the location of plaques
- sensory or motor disturbance
- cranial nerve involvement, e.g. optic neuritis, trigeminal neuralgia
- classification
- clinically isolated syndrome (CIS); isolated neurological deficit with a solitary plaque on imaging; progression to MS is not certain
- relapsing-remitting (RRMS); 70% of cases; on-off periods of symptoms with a full resolution in between flares
- secondary progressive (SPMS); progression of symptoms in RRMS with the deterioration of baseline functioning
- primary progressive (PPMS); progressive deterioration from diagnosis; little or no remission
- depends on the location of plaques
-
pathophysiology
- white matter demyelination
- visible on MRI as plaques of disease
- damage to the myelin sheath surrounding axons
- little or no underlying neuronal damage
- likely autoimmune, cellular-mediated condition
- no unifying cause or trigger
- some genetic and environmental factors 3
- white matter demyelination
-
investigation
- CT may be performed because of focal neurology but is insensitive
- MRI is the investigation of choice
- should be performed with contrast and include the spine
-
treatment
- managed by neurologists in specialist centers
- treatment is focused on slowing progression
- disease-modifying agents and steroids may be used
- multi-disciplinary team involvement is important
- huge psychological burden
Imaging
-
role of imaging
- initial diagnosis
- determine degree of involvement, e.g. spine
- follow up of plaques
-
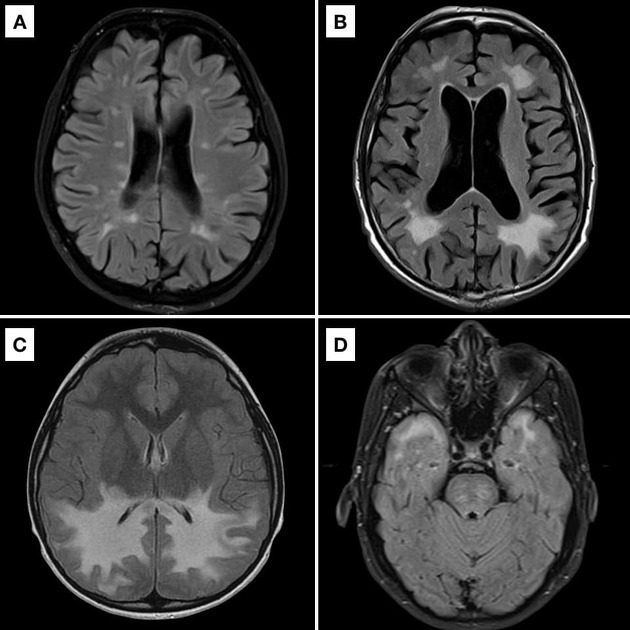
radiographic features
- CT
- not particularly helpful in the assessment of MS
- may be normal
- large plaques may cause edema which can be seen at CT
- active plaques may enhance
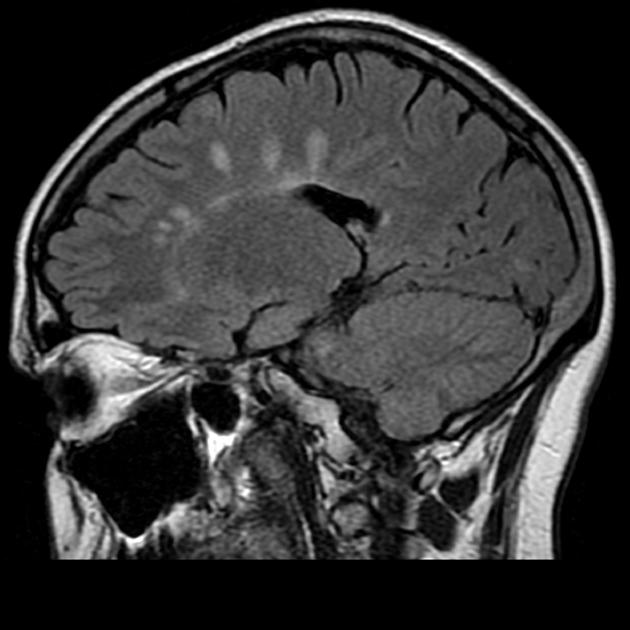
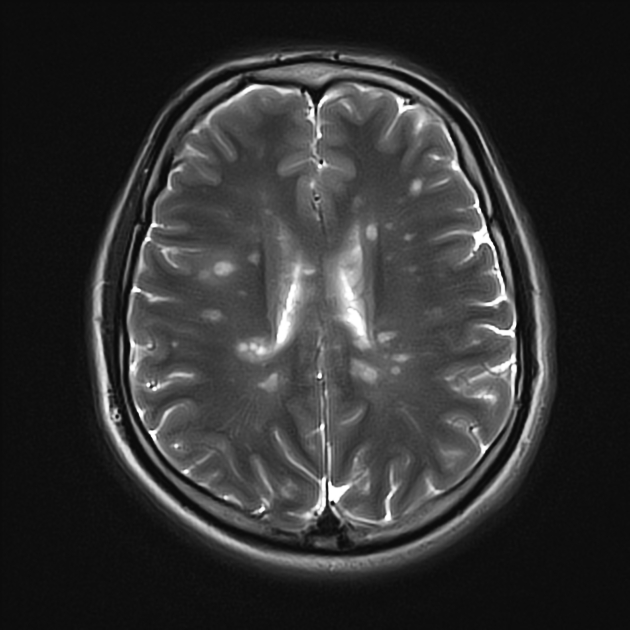
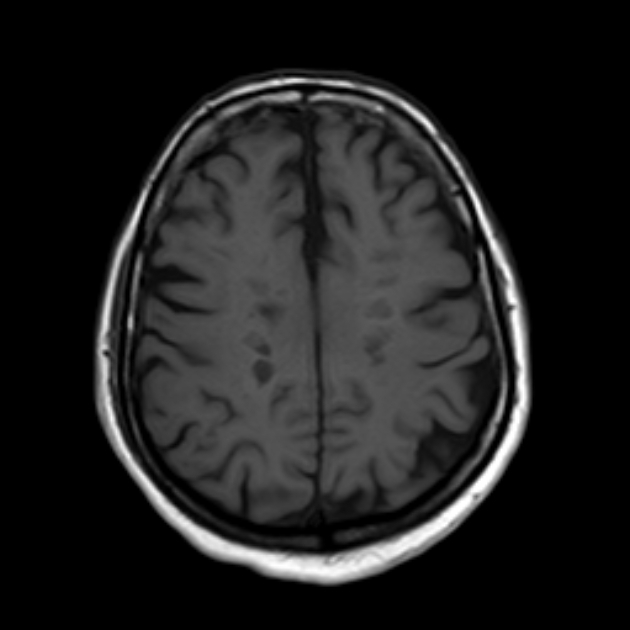
- MRI
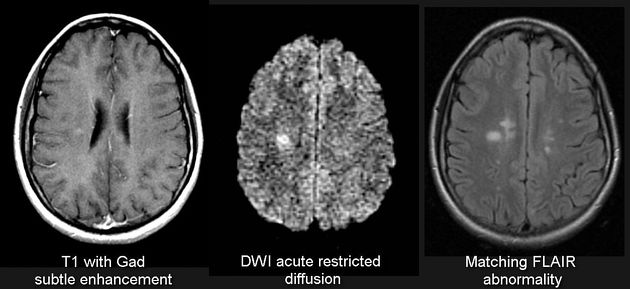
- preferred imaging modailty for diagnosis and follow up
- best visualized on a fluid-sensitive sequence, e.g. T2, FLAIR
- white matter lesions
- characteristic periventricular, they tend to extend perpendicularly and on sagittal views are called "Dawson's fingers" (case 1)
- lesions may occur throughout the CNS and be found in a variety of locations, e.g. juxtacortical, brainstem, cerebellum, or spinal cord (also part of the CNS)
- enhancement is a marker of activity and can be used to determine lesion load and disease progression (case 4)
- limits of conventional MRI technique: it is less sensitive to the associated diffuse damage in normal-appearing white matter.5 In fact, normal-appearing white matter in post-mortem studies of patients with MS - despite retaining myelin - often exhibits chronic injury.6 Advanced MRI techniques such as diffusion tensor imaging (DTI) has shown promise as more specific.
- CT




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.