Nasogastric tube positioning
Citation, DOI, disclosures and article data
At the time the article was created Ian Bickle had no recorded disclosures.
View Ian Bickle's current disclosuresAt the time the article was last revised Arlene Campos had no financial relationships to ineligible companies to disclose.
View Arlene Campos's current disclosures- NG tube position
- NGT position
- Evaluation of nasogastric tube position
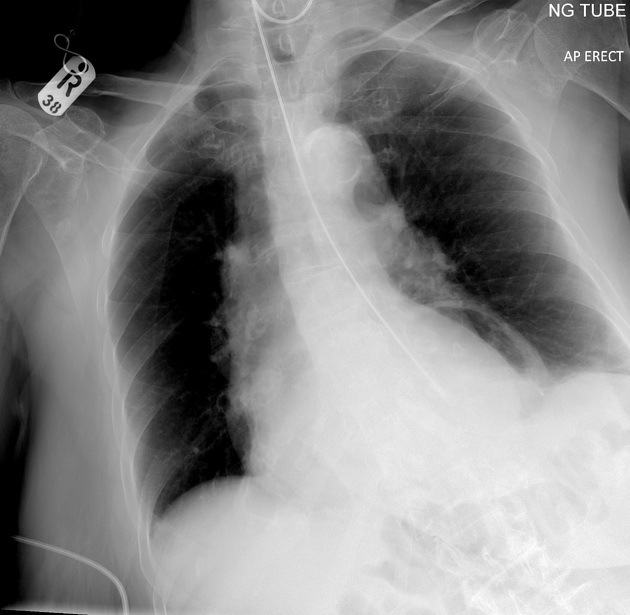
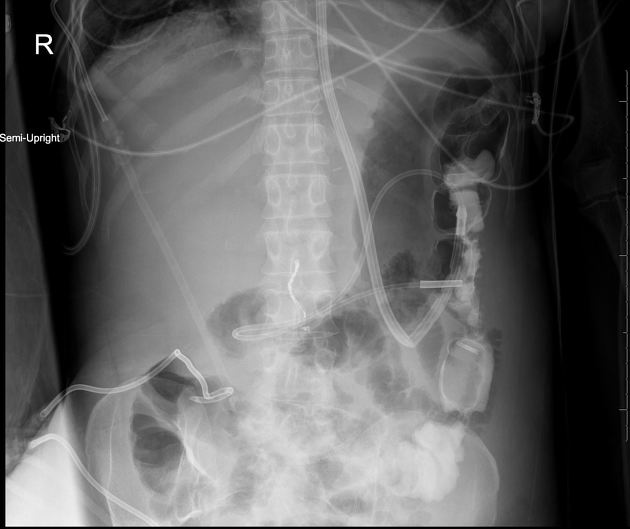
Assessment of nasogastric (NG) tube positioning is a key competency of all doctors as unidentified malpositioning may have dire consequences, including death.
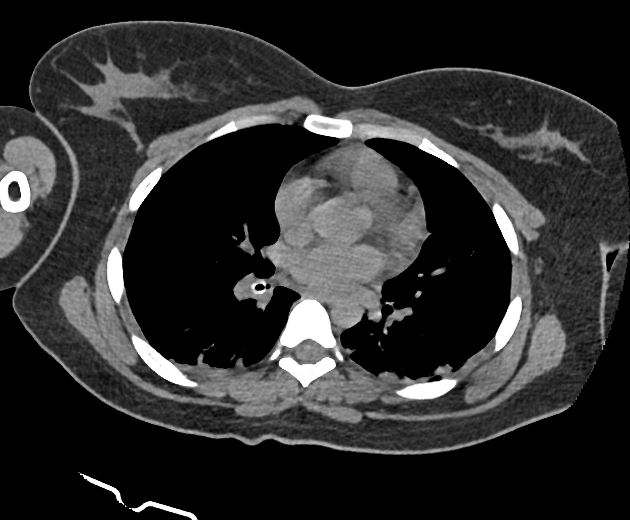
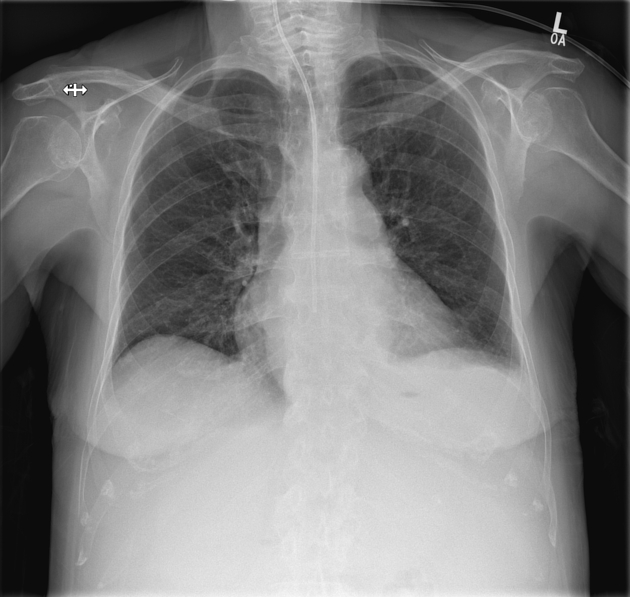
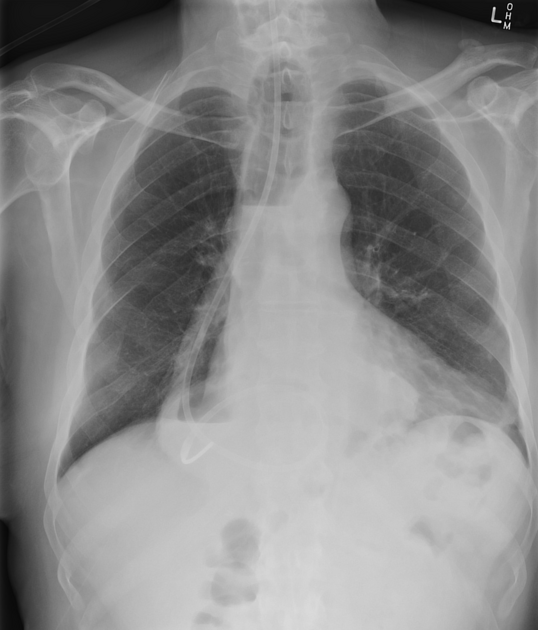
Radiographic features
Plain radiograph
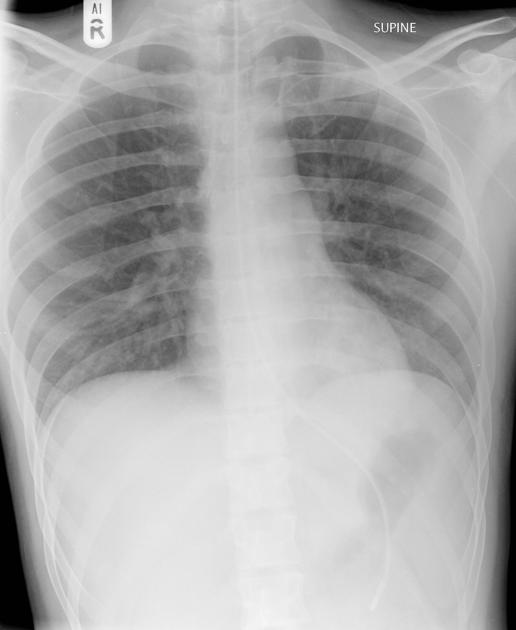
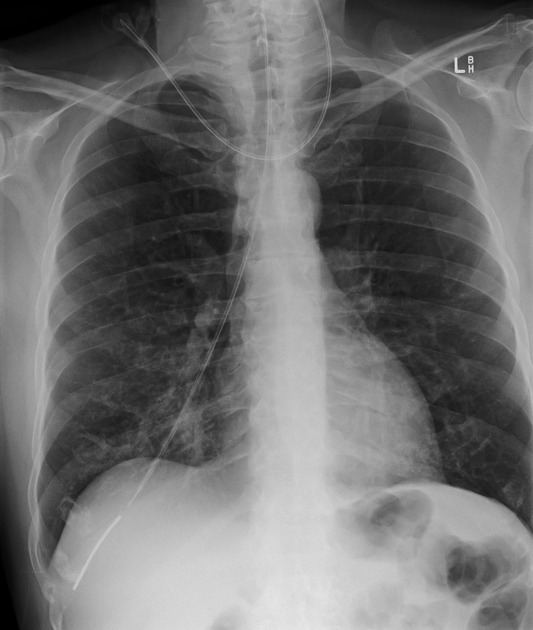
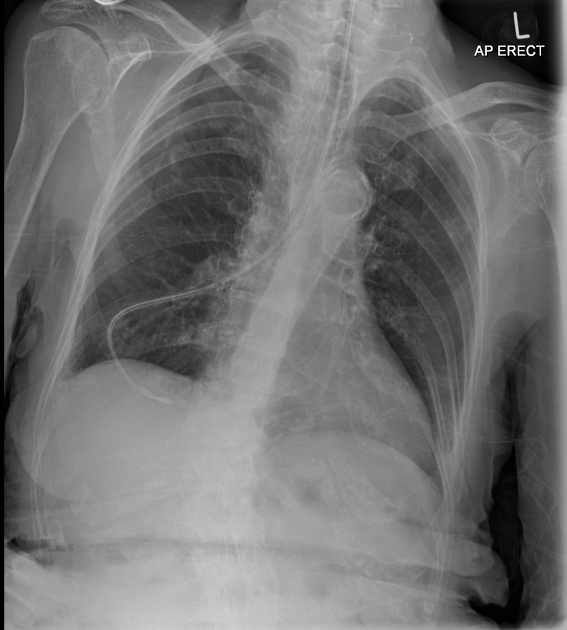
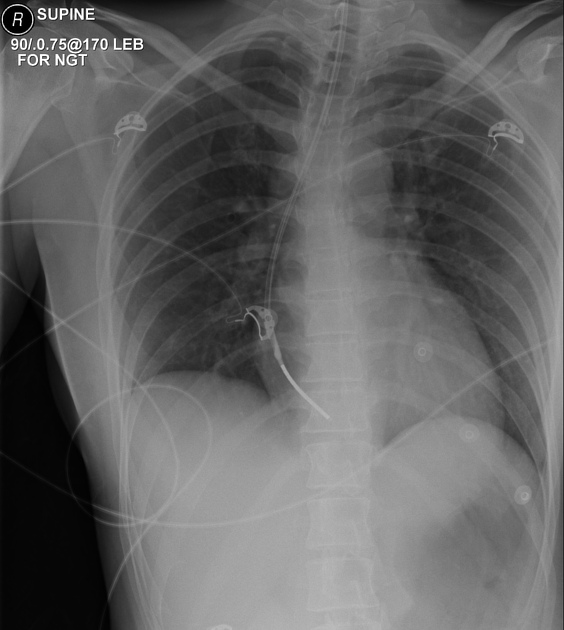
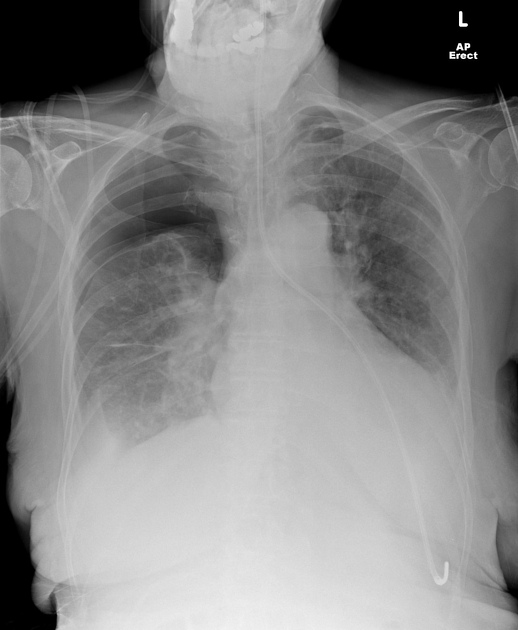
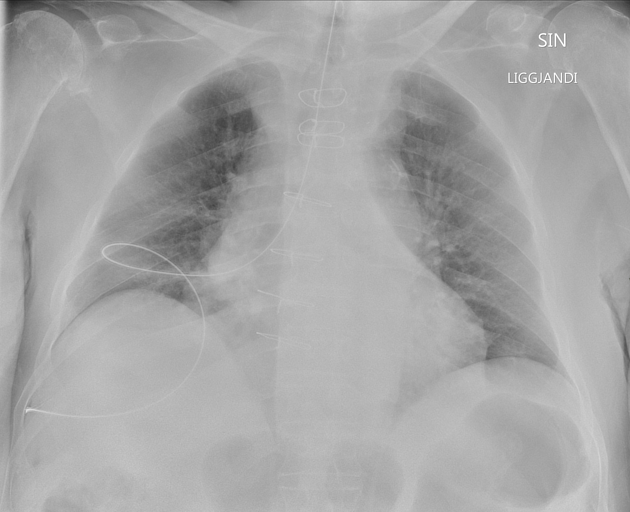
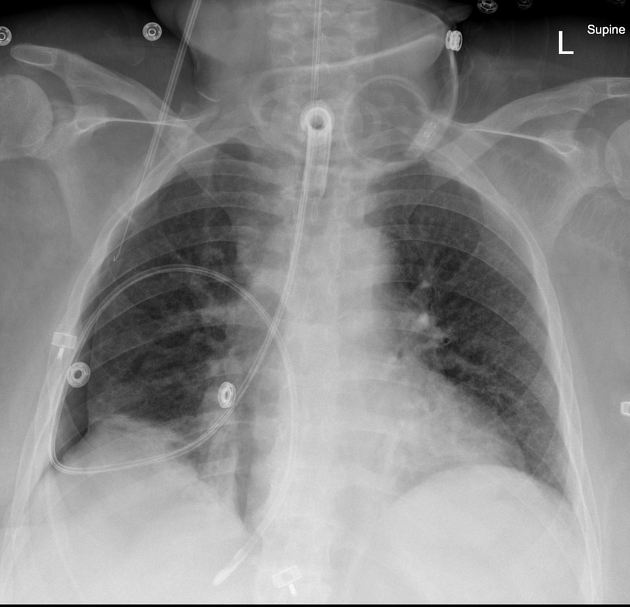
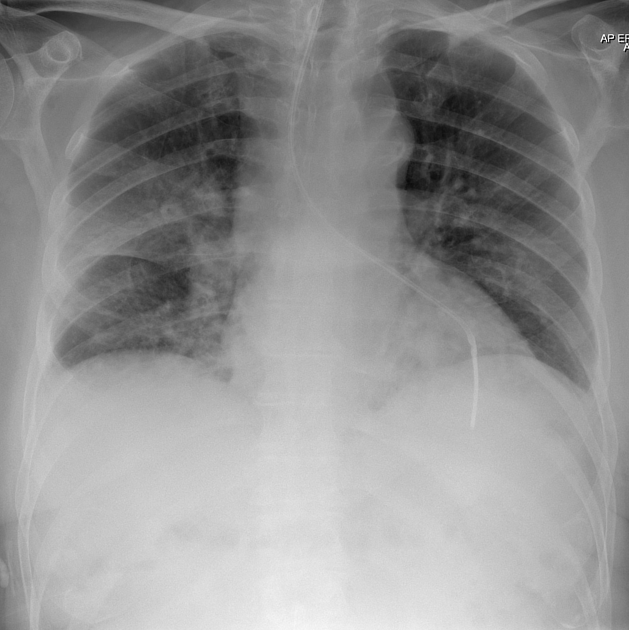
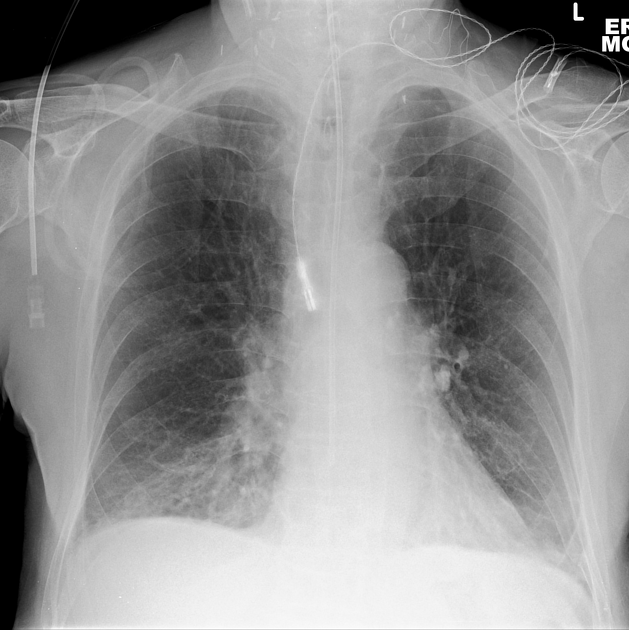
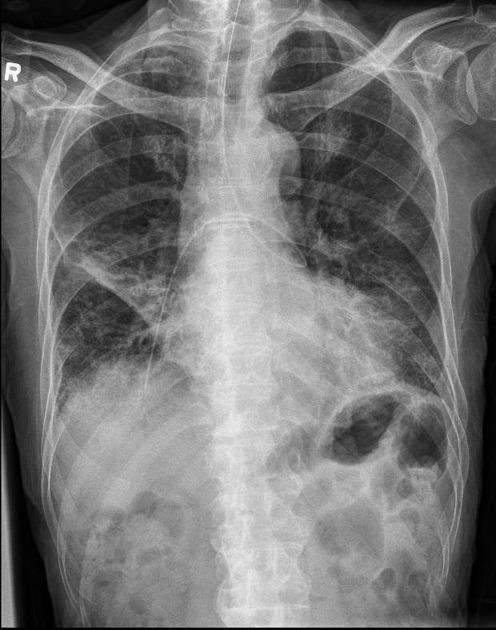
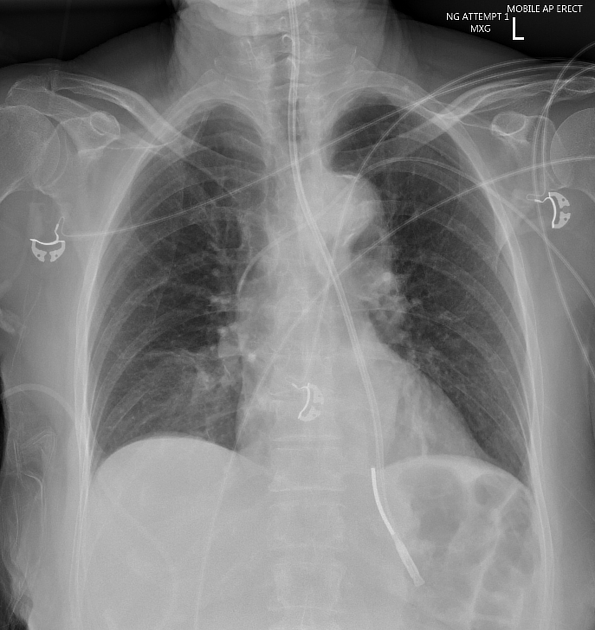
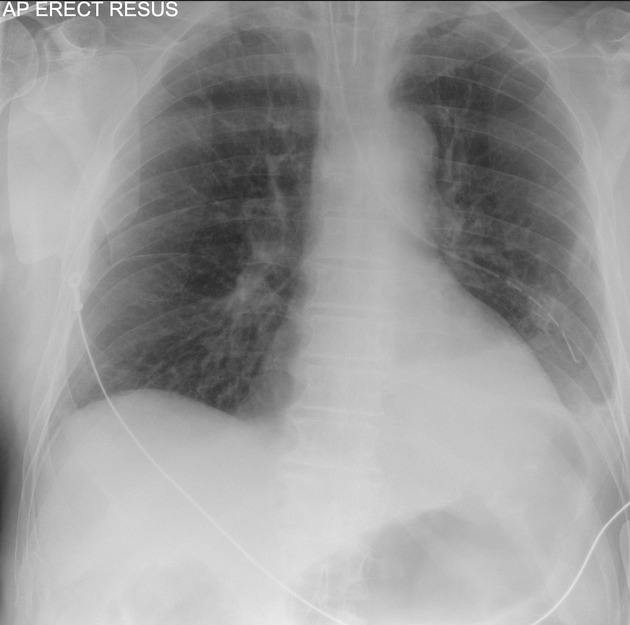
A correctly placed nasogastric tube should 10:
descend in the midline, following the path of the oesophagus and avoiding the contours of the bronchi
clearly bisect the carina or bronchi
cross the diaphragm in the midline
have its tip visible below the left hemidiaphragm
Ideally, the tip should be at least 10 cm beyond the gastro-oesophageal junction 1.
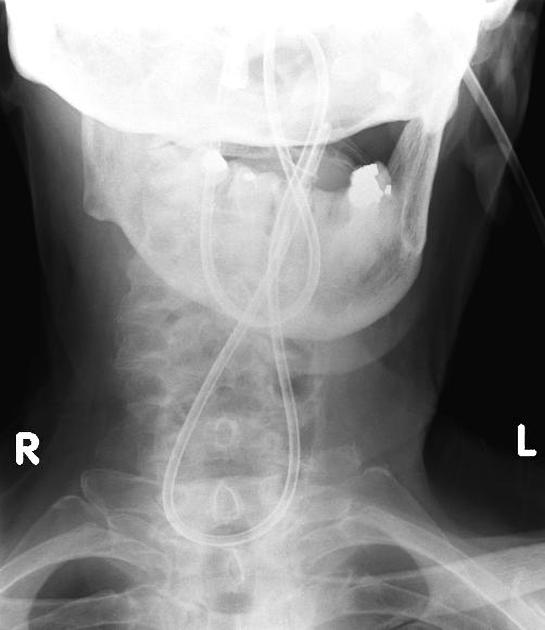
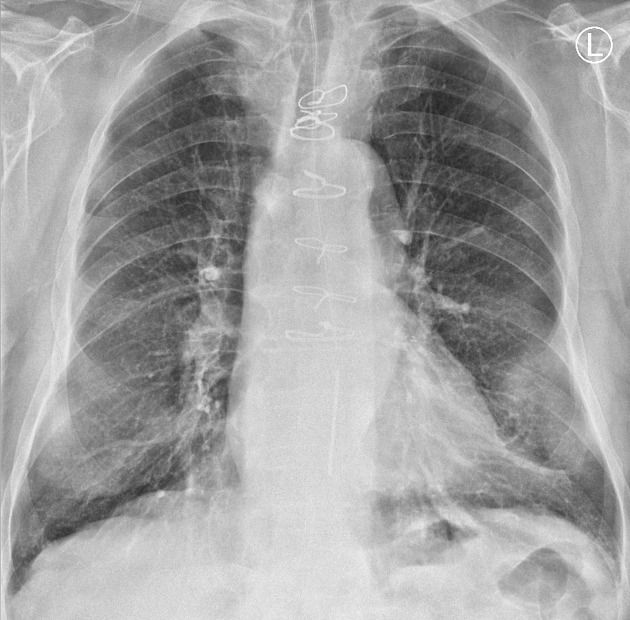
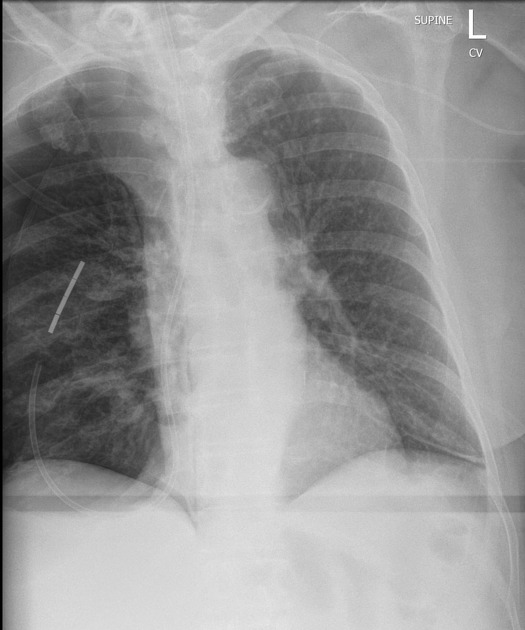
Malpositioning may include tip position:
remaining in the oesophagus
traversing either bronchus or more distally into the lung
coiled in the upper airway
intracranial insertion, possible in both patients with and without skull base trauma or surgery 2
spinal canal insertion is very rare, occurring after skull base surgery in one case report 8,9
In some circumstances fluoroscopic nasojejunal tube insertion is necessary.
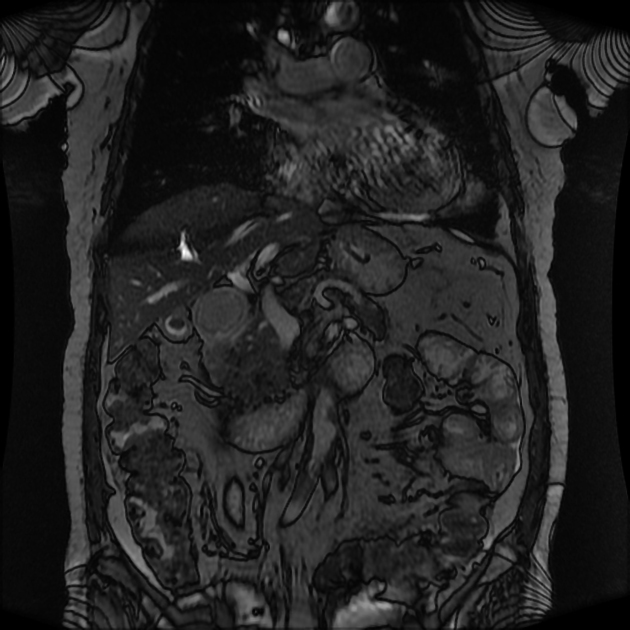
Ultrasound
Point-of-care ultrasonography may be used to guide the nasogastric tube in real-time with the probe placed sequentially in the following locations 7:
-
anterolateral neck
cervical oesophagus typically visualised to the left, posterolateral to the trachea
an intraluminal curvilinear echogenic interface represents oesophageal placement of the tube
-
epigastrium
with a longitudinal view of the gastro-oesophageal junction, the nasogastric tube may be advanced into the stomach under direct visualisation
oblique and sagittal scan planes to view the tube coursing through the gastric fundus and terminating in the antrum, confirming correct placement
Complications
Overall, complications occur in 1-3% of cases, with fatal sequelae in ~0.3% of cases. Complications include 1-6,8,9:
-
upper airway
epistaxis from insertion trauma
-
lower airway
-
enteral
-
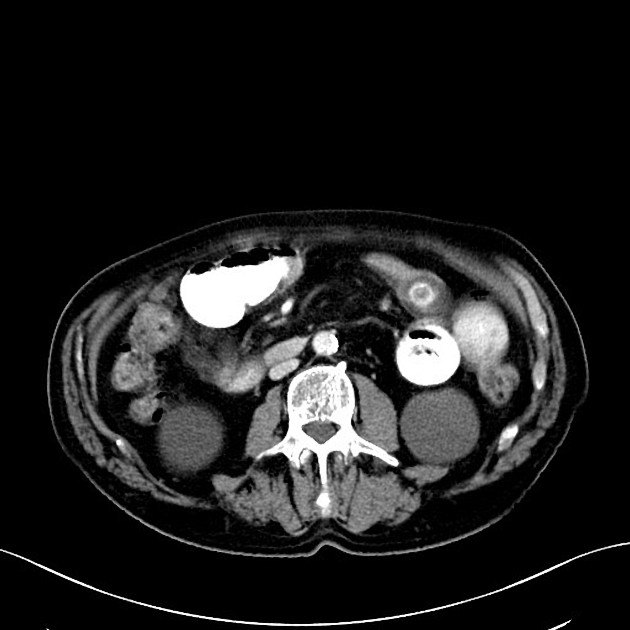
GI perforation and mediastinitis or peritonitis
may further complicate with intravascular placement
GI obstruction
knotting/tangling of the tube
-
-
intracranial and spinal canal
focal neurological deficits
Quiz questions
References
- 1. Pillai JB, Vegas A, Brister S. Thoracic complications of nasogastric tube: review of safe practice. Interact Cardiovasc Thorac Surg. 2005;4 (5): 429-33. doi:10.1510/icvts.2005.109488 - Pubmed citation
- 2. Freij RM, Mullett ST. Inadvertent intracranial insertion of a nasogastric tube in a non-trauma patient. (1997) Journal of accident & emergency medicine. 14 (1): 45-7. Pubmed
- 3. Isik A, Firat D, Peker K, Sayar I, et al. A case report of esophageal perforation: Complication of nasogastric tube placement. (2014) American Journal of Case Reports. 15: 168. doi:10.12659/AJCR.890260 - Pubmed
- 4. Tai CM, Wang HP, Lee CT, et al. Esophageal obstruction by a tangled nasogastric tube. (2010) Gastrointestinal endoscopy. 72 (5): 1057-8. doi:10.1016/j.gie.2010.03.1131 - Pubmed
- 5. Hutchinson R, Ahmed AR, Menzies D. A case of intramural oesophageal dissection secondary to nasogastric tube insertion. (2008) Annals of the Royal College of Surgeons of England. 90 (7): W4-7. doi:10.1308/147870808X303128 - Pubmed
- 6. Duthorn L, Steinberg HS, Hauser H, et al. Accidental Intravascular Placement of a Feeding Tube . (1998) Anesthesiology: The Journal of the American Society of Anesthesiologists. 89 (1): 251.
- 7. Zatelli M, Vezzali N. 4-Point ultrasonography to confirm the correct position of the nasogastric tube in 114 critically ill patients. (2017) Journal of ultrasound. 20 (1): 53-58. doi:10.1007/s40477-016-0219-0 - Pubmed
- 8. Hanna AS, Grindle CR, Patel AA, et al. Inadvertent insertion of nasogastric tube into the brain stem and spinal cord after endoscopic skull base surgery. (2012) American journal of otolaryngology. 33 (1): 178-80. doi:10.1016/j.amjoto.2011.04.001 - Pubmed
- 9. Vahid B. Inadvertent placement of a feeding tube in brainstem and spinal cord. (2007) Internal medicine journal. 37 (8): 577-8. doi:10.1111/j.1445-5994.2007.01410.x - Pubmed
- 10. NHS Improvement, Resource set - Initial placement checks for nasogastric and orogastric tubes. https://improvement.nhs.uk/documents/193/Resource_set_-_Initial_placement_checks_for_NG_tubes_1.pdf
Incoming Links
- Synechiae
- Gastric emphysema
- Oesophageal temperature probe
- Water-soluble contrast challenge
- Pneumothorax
- Chest x-ray - an approach (summary)
- Esophageal balloon tamponade device
- Acute sinusitis
- Medical devices in the thorax
- Lines and tubes (radiograph)
- Gastro-oesophageal junction
- Review areas on chest radiograph
- Nasogastric tube position on chest x-ray (summary)
- Chest radiograph assessment using ABCDEFGHI
- Oesophageal intubation
- Bronchopleural fistula
- Small bowel obstruction
- Oxygen masks
- Nasojejunal tube
- Respiratory distress syndrome and malpositioned UVC
- Venoarterial (VA) ECMO
- Overinflated ETT balloon
- Misplaced nasogastric tube
- Misplaced nasogastric tube
- Nasogastric tube in a large hiatus hernia
- Surfactant deficiency disorder and thermal wrap
- Malpositioned UVC and subacute hepatic fluid collection (TPNoma)
- Misplaced nasogastric tube
- Nasogastric tube in the right lung
- Surfactant deficiency disorder and Broviac line
- Malpositioned UVC and acute hepatic fluid collection (TPNoma)
- Malpositioned PICC and necrotising enterocolitis (NEC)
- Umbilical venous catheter-related hepatic fluid collection (TPNoma) and abscess formation
- Malpositioned nasogastric tube
- Over-the-scope-clip (OTSC)
- Malpositioned nasogastric tube
- Transfusion-related acute lung injury (TRALI)
- Kinked nasogastric tube
Related articles: Chest
- imaging techniques
-
chest radiograph
- radiography
-
approach
- ABCDE
- ABCDEFGHI
- congenital heart disease
- medical devices in the thorax
- common lines and tubes
- nasogastric tubes
- endotracheal tubes
- central venous catheters
- oesophageal temperature probe
- tracheostomy tube
- pleural catheters
- cardiac conduction devices
- prosthetic heart valve
- review areas
-
airspace opacification
- differential diagnoses of airspace opacification
- lobar consolidation
-
atelectasis
- mechanism-based
- morphology-based
- lobar lung collapse
- chest x-ray in the exam setting
- cardiomediastinal contour
- chest radiograph zones
- tracheal air column
- fissures
- normal chest x-ray appearance of the diaphragm
- nipple shadow
-
lines and stripes
- anterior junction line
- posterior junction line
- right paratracheal stripe
- left paratracheal stripe
- posterior tracheal stripe/tracheo-oesophageal stripe
- posterior wall of bronchus intermedius
- right paraspinal line
- left paraspinal line
- aortic-pulmonary stripe
- aortopulmonary window
- azygo-oesophageal recess
- spaces
- signs
- air bronchogram
- big rib sign
- Chang sign
- Chen sign
- coin lesion
- continuous diaphragm sign
- dense hilum sign
- double contour sign
- egg-on-a-string sign
- extrapleural sign
- finger in glove sign
- flat waist sign
- Fleischner sign
- ginkgo leaf sign
- Golden S sign
- Hampton hump
- haystack sign
- hilum convergence sign
- hilum overlay sign
- Hoffman-Rigler sign
- holly leaf sign
- incomplete border sign
- juxtaphrenic peak sign
- Kirklin sign
- medial stripe sign
- melting ice cube sign
- more black sign
- Naclerio V sign
- Palla sign
- pericardial fat tag sign
- Shmoo sign
- silhouette sign
- snowman sign
- spinnaker sign
- steeple sign
- straight left heart border sign
- third mogul sign
- tram-track sign
- walking man sign
- water bottle sign
- wave sign
- Westermark sign
- HRCT
-
chest radiograph
- airways
- bronchitis
- small airways disease
-
bronchiectasis
- broncho-arterial ratio
- related conditions
- differentials by distribution
- narrowing
-
tracheal stenosis
- diffuse tracheal narrowing (differential)
-
bronchial stenosis
- diffuse airway narrowing (differential)
-
tracheal stenosis
- diverticula
- pulmonary oedema
-
interstitial lung disease (ILD)
- Anti-Jo-1 antibody-positive interstitial lung disease
- drug-induced interstitial lung disease
-
hypersensitivity pneumonitis
- acute hypersensitivity pneumonitis
- subacute hypersensitivity pneumonitis
- chronic hypersensitivity pneumonitis
- aetiology
- bird fancier's lung: pigeon fancier's lung
- farmer's lung
- cheese workers' lung
- bagassosis
- mushroom worker’s lung
- malt worker’s lung
- maple bark disease
- hot tub lung
- wine maker’s lung
- woodsman’s disease
- thatched roof lung
- tobacco grower’s lung
- potato riddler’s lung
- summer-type pneumonitis
- dry rot lung
- machine operator’s lung
- humidifier lung
- shower curtain disease
- furrier’s lung
- miller’s lung
- lycoperdonosis
- saxophone lung
-
idiopathic interstitial pneumonia (mnemonic)
- acute interstitial pneumonia (AIP)
- cryptogenic organising pneumonia (COP)
- desquamative interstitial pneumonia (DIP)
- non-specific interstitial pneumonia (NSIP)
- idiopathic pleuroparenchymal fibroelastosis
- lymphoid interstitial pneumonia (LIP)
- respiratory bronchiolitis–associated interstitial lung disease (RB-ILD)
- usual interstitial pneumonia / idiopathic pulmonary fibrosis (UIP/IPF)
-
pneumoconioses
- fibrotic
- non-fibrotic
-
lung cancer
-
non-small-cell lung cancer
-
adenocarcinoma
- pre-invasive tumours
- minimally invasive tumours
- invasive tumours
- variants of invasive carcinoma
- described imaging features
- adenosquamous carcinoma
- large cell carcinoma
- primary sarcomatoid carcinoma of the lung
- squamous cell carcinoma
- salivary gland-type tumours
-
adenocarcinoma
- pulmonary neuroendocrine tumours
- preinvasive lesions
-
lung cancer invasion patterns
- tumour spread through air spaces (STAS)
- presence of non-lepidic patterns such as acinar, papillary, solid, or micropapillary
- myofibroblastic stroma associated with invasive tumour cells
- pleural invasion
- vascular invasion
- tumours by location
- benign neoplasms
- pulmonary metastases
- lung cancer screening
- lung cancer staging
-
non-small-cell lung cancer













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.