Craniocerebral neuroblastoma metastases usually involve the calvaria, orbits, skull base and dura.
This should not be confused with primary CNS neuroblastoma, FOXR2-activated that, in contrast, usually arise from the cerebral hemispheres 5.
Please refer to the article neuroblastoma for a general discussion on this entity.
On this page:
Epidemiology
The epidemiology of neuroblastoma is discussed in the parent article (see neuroblastoma). It is worth noting, however, that in children, the spread of systemic neuroblastoma is the most common cause of orbital metastases 4.
Clinical presentation
The clinical presentation will depend upon the location of metastases, usually presenting with mass effect. Presentation, therefore includes:
- proptosis
- periorbital ecchymosis ("racoon eyes")
- palpable calvarial masses
Radiographic features
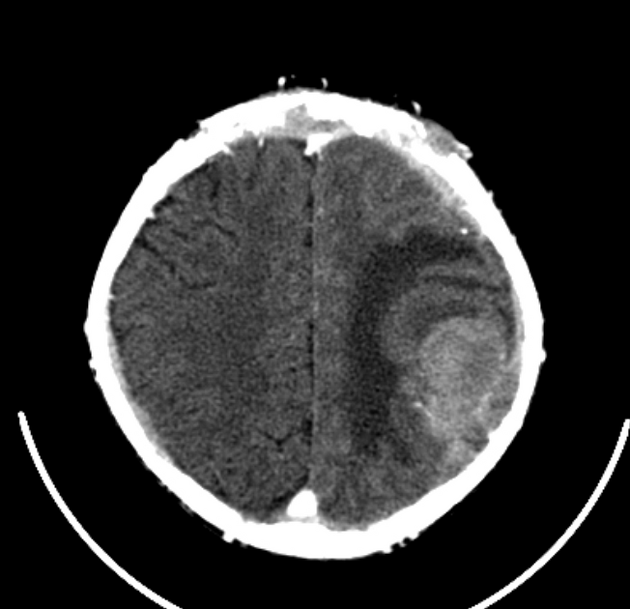
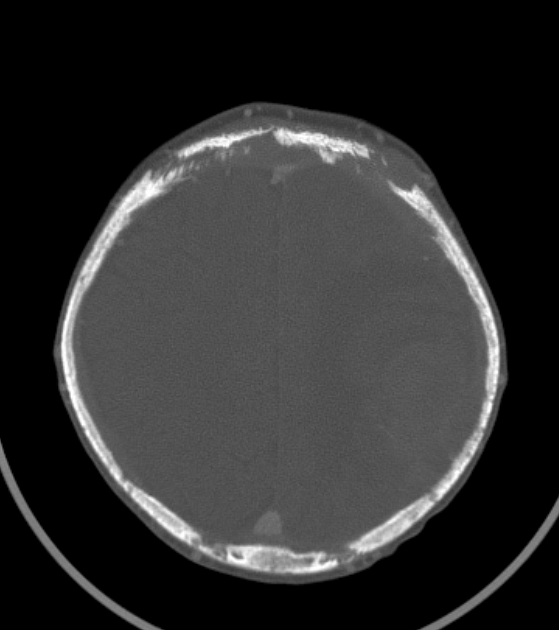
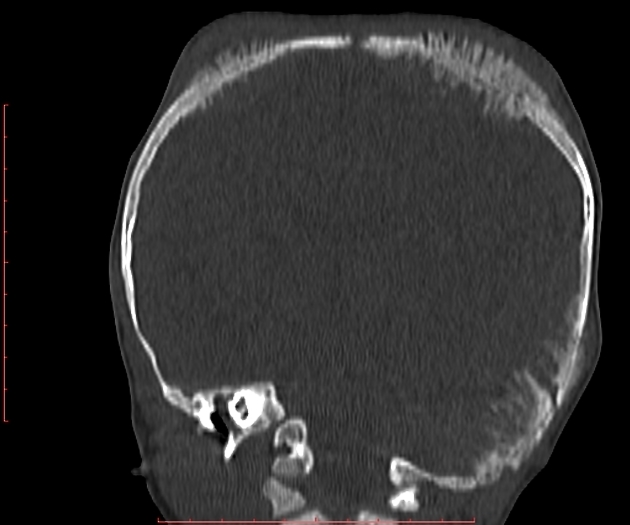
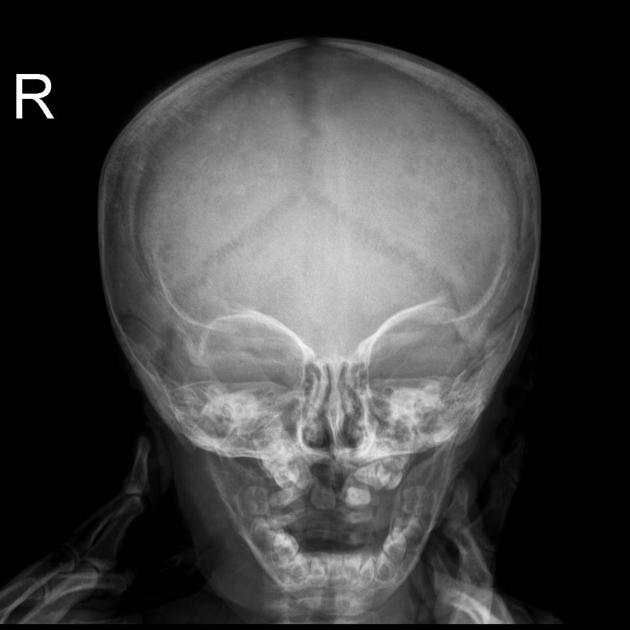
CT
- spiculated periorbital bone mass, typically involving the roof or lateral wall/sphenoid wings
- "hair on end" spiculated periostitis of orbits and skull usually associated with bone destruction
- sutural separation: non-uniform sutural separation with indistinct suture margins
- cranial metastases are nearly always extradural (may mimic epidural or subdural hematoma)
MRI
- T1: hypointense to muscles
- T2: heterogeneous usually hyperintense to muscles
- T1 C+ (Gd): vigorously enhances, may be heterogeneous
- MRV: may narrow or invade adjacent dural sinuses
Nuclear medicine
- MIBG (meta-iodo benzyl guanidine): avid uptake by neural crest tumors
- TC-99-m-MDP: shows increased uptake due to the calcium metabolism of the tumor
- PET: shows high sensitivity and specificity for recurrent tumors
Differential diagnosis
Imaging differential considerations include:
- consider intracranial metastases from
- leukemia
- dural or calvarial based masses
- usually associated with intraparenchymal masses
- Ewing sarcoma
- osteosarcoma
- skeletal involvement with Langerhans cell histiocytosis: lytic bone lesions without periosteal bone formation
- extra-axial intracranial hematoma







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.