Osteoradionecrosis (ORN) refers to a severe delayed radiation-induced injury and is characterized by bone tissue necrosis and failure in healing.
On this page:
Terminology
There is some overlap with the terms radiation osteitis and radio-osteonecrosis. The condition most often occurs after radiotherapy and then might be referred to as post-radiotherapyosteonecrosis 13.
Pathology
Two main theories exist to describe the pathogenesis of ORN. Neither has been proven outright, and instead are often seen as complementary to one another.
Marx's theory, or hypoxic-hypocellular-hypovascular theory was first proposed in 1983 and describes a process of radiation induced hypovascularity, hypoxia and hypocellularity 14. This theory provides the rationale for hyperbaric oxygen therapy.
The fibroatrophic theory was first proposed by Delanian in 2004 and suggests that radiation damage induces fibroblast dysregulation leading to inability to repair tissue damage 15. This theory provides the rationale for antioxidant and anti fibrotic therapies.
Usually, large radiation doses are required for osteoradionecrosis to occur (e.g. <3000-5000 cGy) 2.
Location
While it can involve any bone within the irradiated field, there are specific sites in which osteoradionecrosis is more commonly seen. These include:
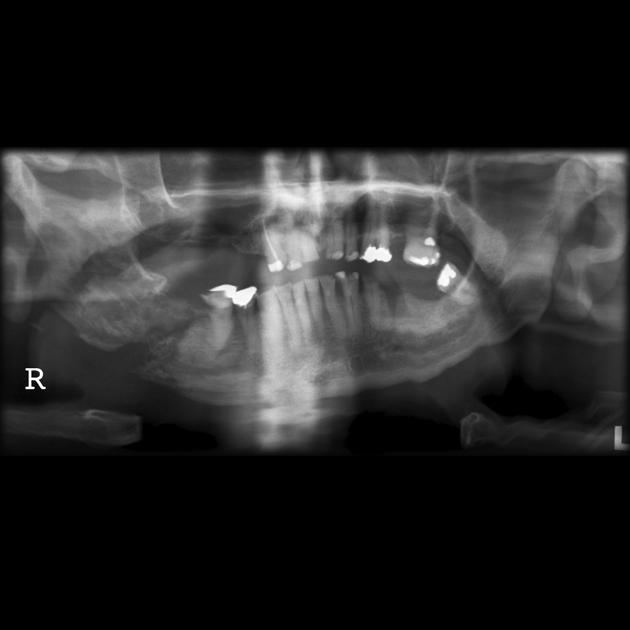
mandible: mandibular osteoradionecrosis: this site is particularly prone due to its superficial location and high doses of radiation required to radically treat naso-oropharyngeal tumors
chest wall-shoulder-humerus-scapula
spine
bony pelvis
Radiographic features
While there are general features, radiographic features can somewhat vary with the site of involvement.
Plain radiograph
With mandibular osteoradionecrosis, there can be ill-defined cortical destruction without sequestration. In osteoradionecrosis of the ribs, clavicle, scapula, and humerus, radiography may demonstrate 2 :
osteopenia: typically occurs after ~1 year postirradiation 4
disorganization and coarsening of trabecular architecture
cortical irregularity
heterogenous bone density
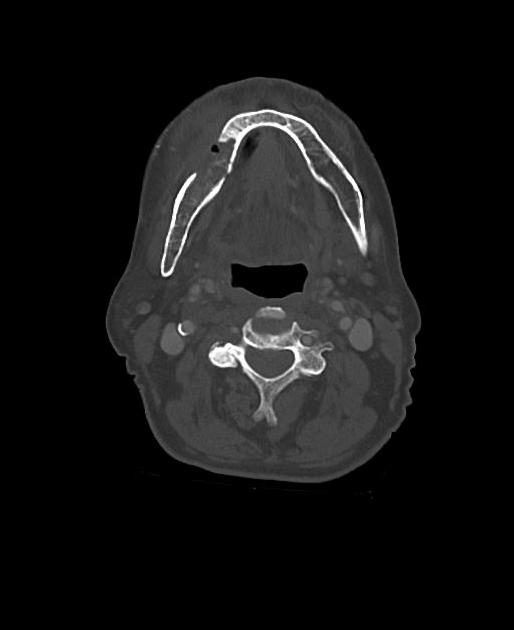
CT
With mandibular osteoradionecrosis, CT may additionally show cortical interruptions and loss of spongiosa trabeculation 6. In other sites, CT may show the presence of subtle fractures, alterations in bone architecture and dystrophic soft-tissue calcification.
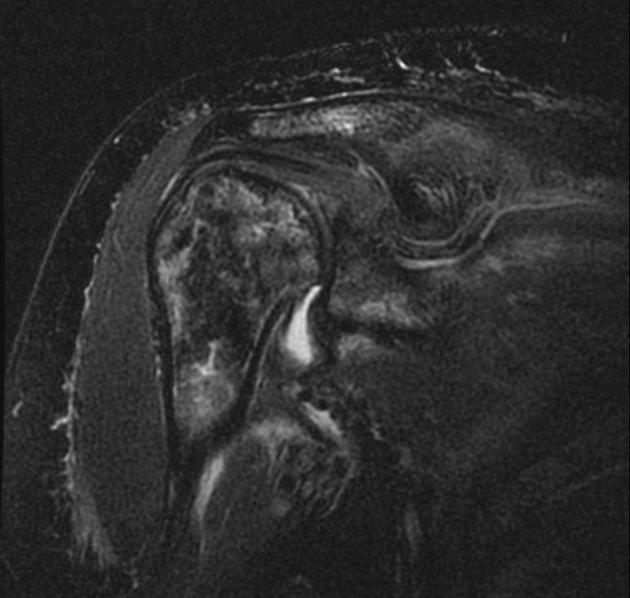
MRI
On MRI, they can be the development of new heterogeneous signal within the marrow of an irradiated area (intermediate or low T1 signal, intermediate or high T2 signal). Osteoradionecrosis with or without osteomyelitis can be extremely difficult to differentiate from a recurrent tumor. Adjacent muscles may appear edematous and show intense enhancement, which can be difficult to differentiate from recurrent tumor if bone changes are not visible on CT 10.
In osteoradionecrosis of the spine, hematopoietic cellular elements of the spinal marrow can also be replaced with fat, which then has 2
T1: high signal intensity
T2: intermediate signal intensity
Staging
Multiple staging criteria exist with varying utility. Clinical features, radiological findings and response to treatment all factor in to differing degrees depending upon the chosen criteria. The below list is not exhaustive.
Store and Boysen 11:
Stage 0 = mucosal defects only
Stage I = radiological evidence of ORN + intact mucosa
Stage II = radiologic evidence of ORN + denuded bone
Stage III = radiologic evidence of ORN + exposed bone + extra oral fistula + infection
Modified Marx 12:
Stage I = exposed alveolar bone + responds to hyperbaric oxygen (HBO)
Stage II = does not respond to HBO, requires sequestrectomy/ saucerisation
Stage III = full thickness bone damage and/or pathologic fracture/ fistula. Often requires complete resection.
Treatment and prognosis
The condition either stabilizes or gradually worsens, which then becomes notoriously difficult to manage.
Differential diagnosis
To give a meaningful differentiation, location and imaging modality needs to be taken into account. General differential consideration includes:
original tumor recurrence
radiation-induced secondary tumor e.g. sarcoma
complicating infection: osteomyelitis (can also be an association) 10






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.