Ovarian torsion occurs when the ovary rotates around its supporting ligaments, twisting and compressing the accompanying blood vessels and lymphatics. The term adnexal torsion is preferred because a portion of the fallopian tube is commonly torsed along with the ovary. The term adnexal torsion also encompasses rarer entities that do not affect the ovaries such as isolated torsion of the fallopian tube and torsion of paratubal, broad ligament and paraovarian cysts.
The diagnosis is commonly missed, which leads to delayed surgery and complications.
On this page:
Epidemiology
The true incidence of adnexal torsion is unknown. One estimate suggests that up to 3% of women presenting to an emergency department with acute abdominal pain have ovarian torsion 24. Although most cases occur during reproductive years the age range extends from prenatal to postmenopausal 25.
Clinical presentation
Patients typically present with sudden severe pelvic pain, either intermittent or sustained. Often patients report similar episodes during the previous month. Sometimes there is a history of vigorous activity. Confusingly, pain can radiate to the flank, groin and back.
Nausea typically coincides with the onset of pain and vomiting may follow. Nausea and/or vomiting accompanying pain are helpful clues to the diagnosis in 85% of cases. Leukocytosis and fever are common and may indicate necrosis.
Tenderness may be focal, diffuse or not apparent.
Ovarian torsion has an increased incidence throughout pregnancy and the post-partum period, but especially between 10-17 weeks gestation, related to persistent corpus luteum cysts.
Ovarian torsion has been observed in the fetus and if a cyst is present it can be drained in utero. Clinical features in small children are typically nonspecific, such as vomiting and restlessness. Pain may be diffuse.
Pathology
The ovary is mobile, suspended by the infundibulopelvic (suspensory) and utero-ovarian ligaments. The ovary has dual blood supply, primarily from the ovarian vessels in the infundibulopelvic ligament, and these anastomose with uterine artery branches in the utero-ovarian ligament. Torsion occurs when the ovary twists around these ligaments. Lymphatic, venous and arterial obstruction varies according to the number and tightness of the twists. Lymphatic and venous occlusion causes central ovarian edema which further compromises arterial inflow. Hemorrhagic infarction can follow within hours.
Over 85% of cases are associated with ovarian enlargement (5-30 cm) due to a mass or cyst(s) caused by:
ovulation induction (multicystic ovaries or hyperstimulation)
benign mass, commonly mature cystic teratoma or adnexal cysts
Endometrioma, tubo-ovarian abscess and malignancy are more likely to have pelvic adhesions and are less likely to tort. However malignant tumors may account for 3-20% of cases of torsion in postmenopausal women.
Hypermobility of the ovary due to relatively lax ligaments may be a factor in children and teens.
Isolated tubal torsion is predisposed by hydrosalpinx, hematosalpinx, paratubal cyst, ectopic pregnancy or elongated mesosalpinx with a tortuous tube 23.
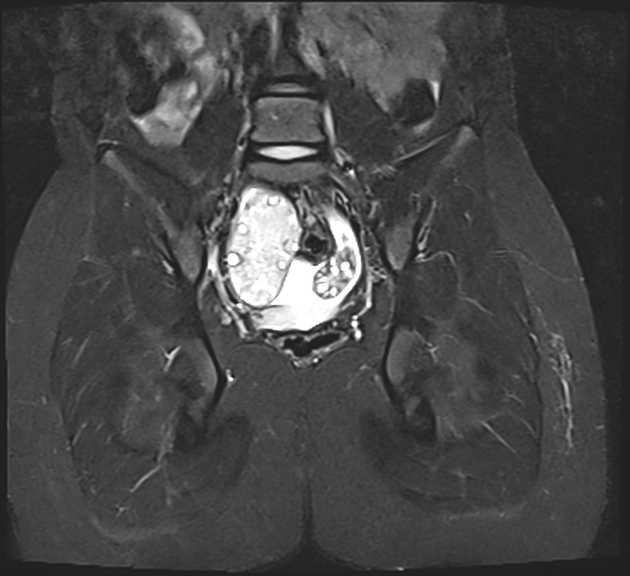
Radiographic features
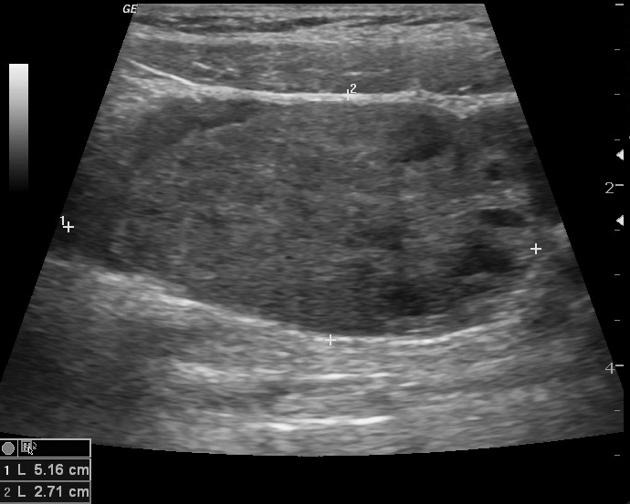
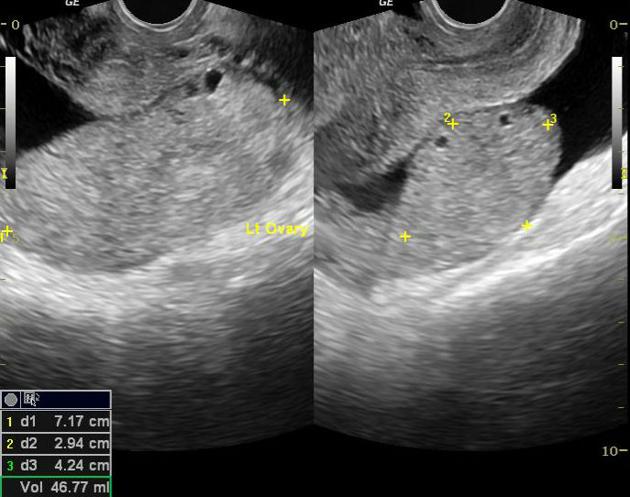
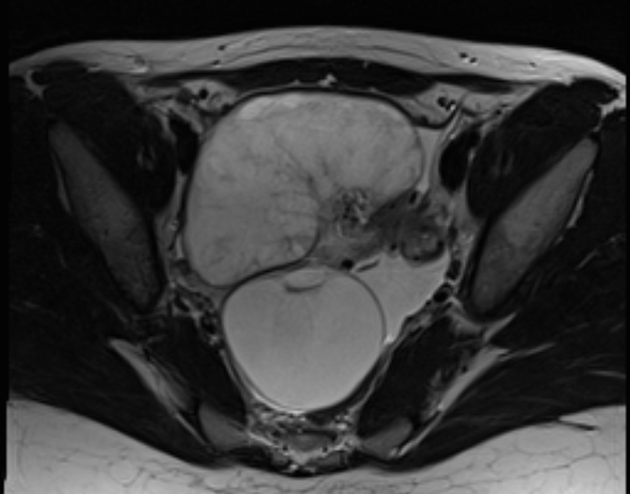
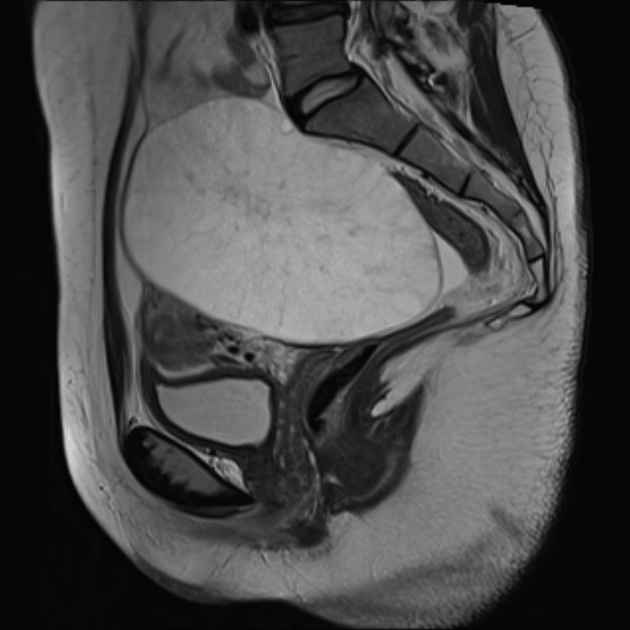
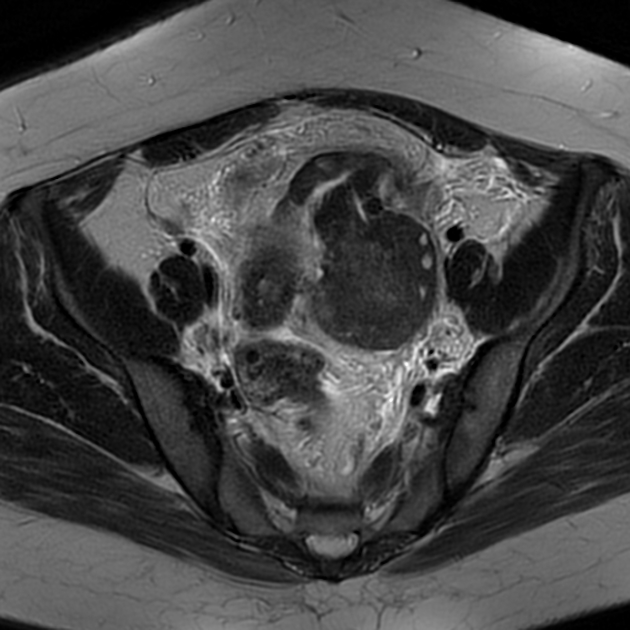
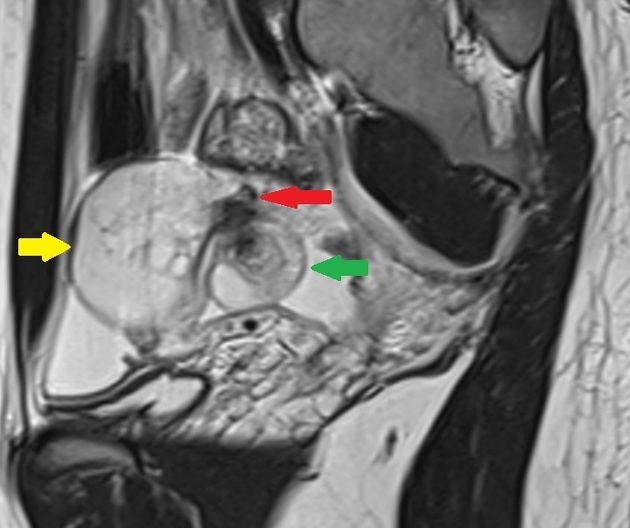
The key features of torsion are ovarian edema and swelling due to venous and lymphatic engorgement. This exacerbates arterial compromise and can cause hemorrhage and infarction. A normal ovary measures approximately 4 x 2 x 3 cm with a volume of 9.8 cc. Following ovarian torsion a maximum diameter >5 cm is 89% sensitive 21.
Additional concurrent imaging characteristics indicating adnexal torsion include:
rounded/spherical ovarian shape ref
torsed ovary shifts towards the midline 26,27 to lie anterior or posterior to the uterus
uterus is deviated towards the torsed ovary 26,27
twisted vascular pedicle may be apparent as a layered “whirlpool” structure between the uterus and ovary comprising fallopian tube, mesosalpinx and vessels ref
edema fluid expands the central stroma, displacing the follicles peripherally 26,27
distended fallopian tube 26,27
peritoneal free fluid 26,27
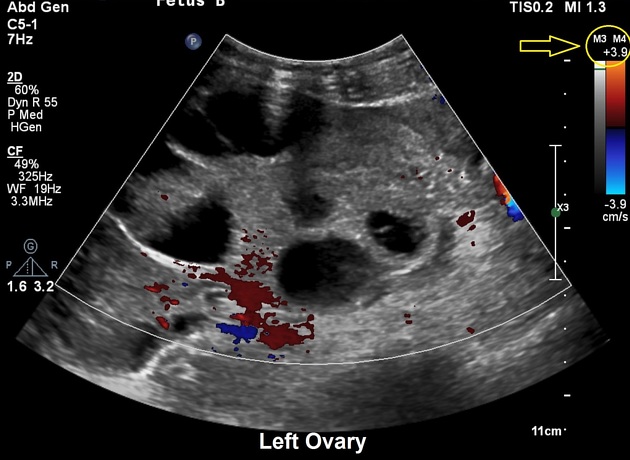
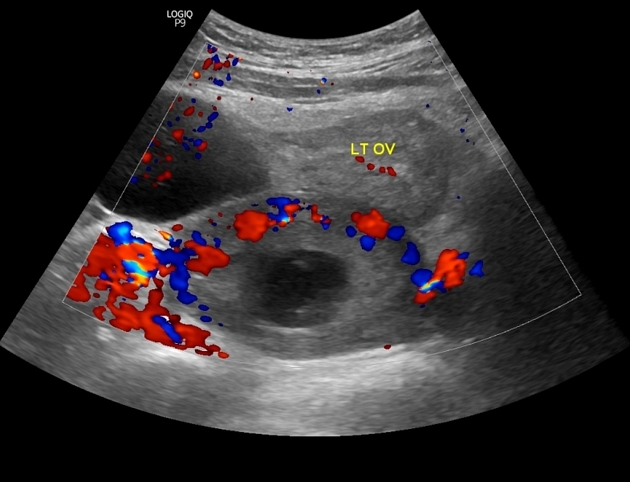
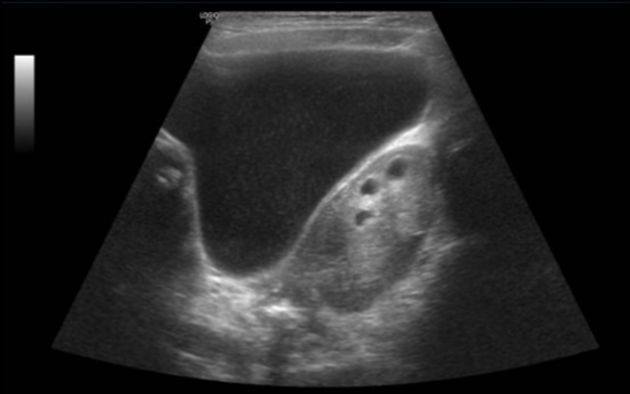
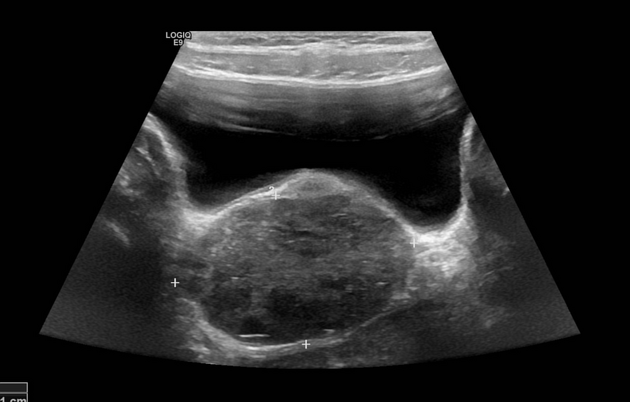
Ultrasound
Ultrasound is the initial imaging modality of choice. Sonographic features include:
enlarged edematous globular ovary is the key finding 17
ovary >5 cm in maximum diameter or >20 cc in volume
rarely normal size ovaries (isolated fallopian tube or paraovarian cyst torsion)
stromal hypoechogenicity (edema) or patchy hyperechogenicity (hemorrhage)
cystic or hemorrhagic degeneration (indicates established infarction)
peripheral follicles surrounded by a hyperechoic ring (follicular ring sign) most likely due to hemorrhage in the thecal layer
unusual ovarian location e.g. anterior or posterior to the uterus, or a change in position
tilted uterus (pulled by the twisted ligaments)
-
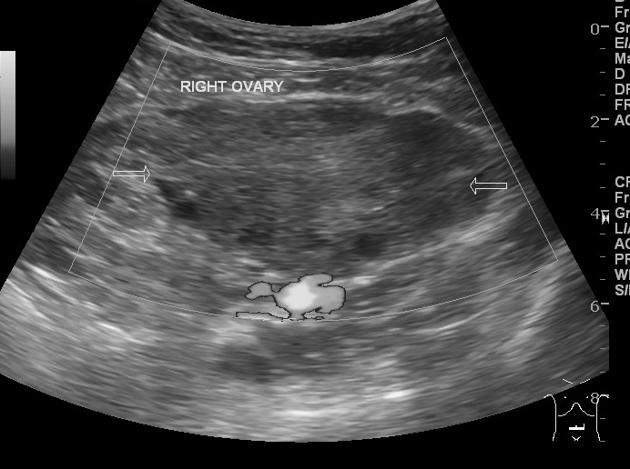
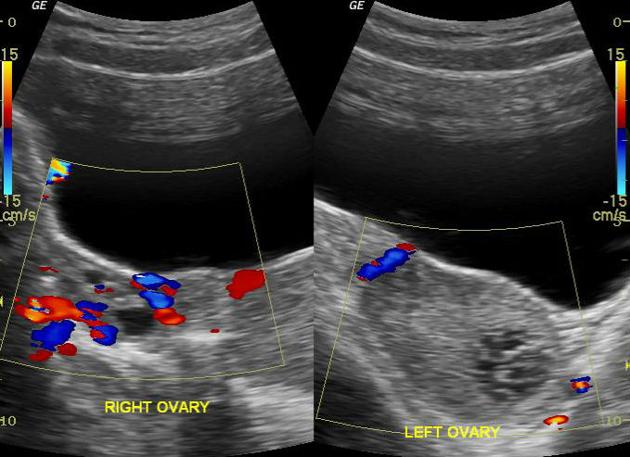
Doppler findings in torsion are variable:
little or no ovarian venous flow (sensitivity of 100% and specificity of 97%) 14
absent arterial flow (less common, poor prognosis)
absent or reversed diastolic flow
asymmetrical flow compared to normal ovary
normal vascularity (due to intermittent torsion or good collateral flow)
whirlpool sign of twisted vascular pedicle 3 is pathognomonic and is helpful in cases with normal Doppler flow with sensitivity of about 90%
an underlying ovarian lesion may be seen (lead point for torsion)
ovary tenderness to transducer pressure 13
free pelvic fluid may be seen in >80% of cases
Isolated fallopian tube torsion is rare and the findings may include tubal dilatation tapering at each end (beak sign) with thick echogenic walls.
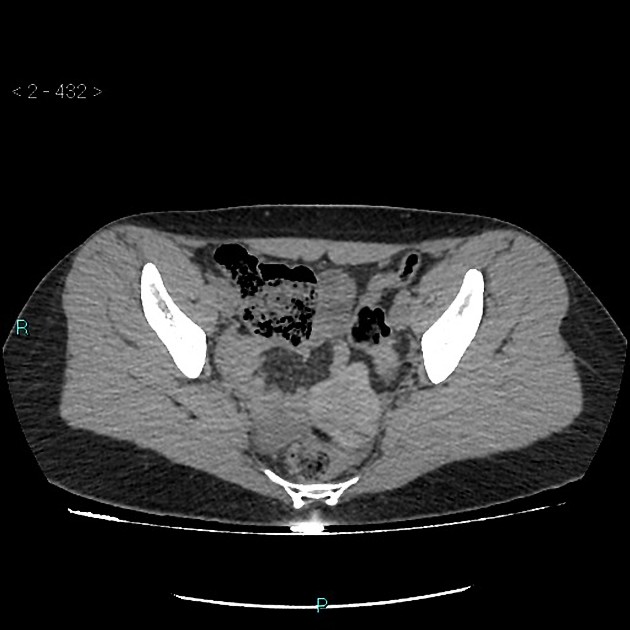
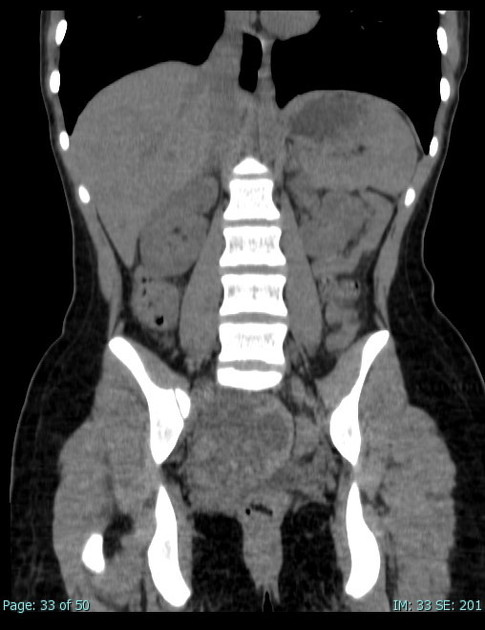
CT
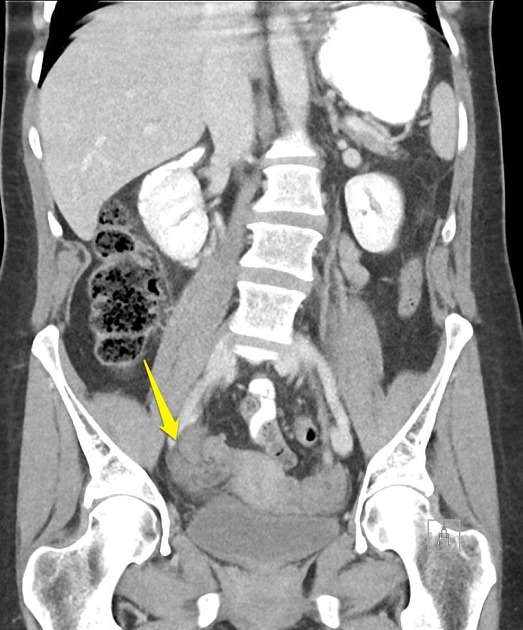
If the clinical features are nonspecific CT may be the first investigation, and although not ideal there are features that favor ovarian torsion:
edematous or hemorrhagic mass anterior or posterior to the uterus (which may be tilted), with patchy enhancement and adjacent free fluid
peripheral follicles (string of pearls), if present, indicate ovarian origin
mass (e.g. cyst or mature teratoma)
soft tissue, vessels +/- fat at the anterolateral margin of the uterus can suggest a twisted pedicle 11
fat stranding in the adnexa (non-specific)
Hemorrhage is a sign of potential necrosis. Heterogeneous increased attenuation on non-enhanced CT may indicate hemorrhage whereas heterogeneous attenuation on enhanced CT may indicate either patchy hemorrhage or diminished vascularity. Whatever the underlying cause, these appearances are a relatively poor prognostic sign.
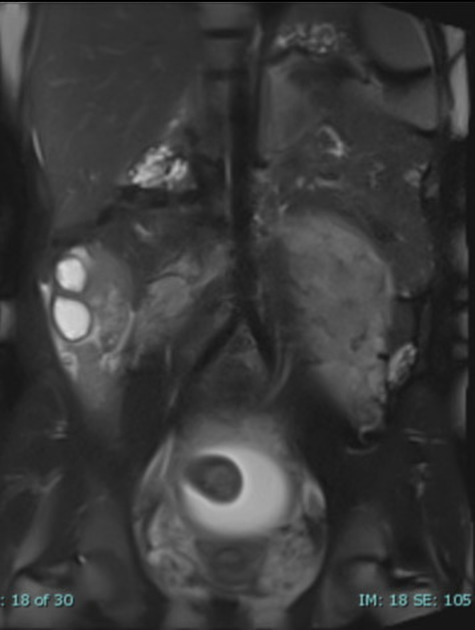
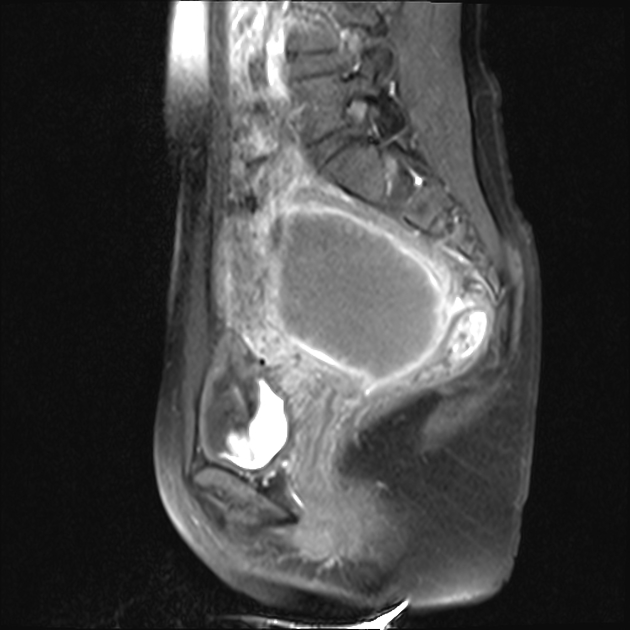
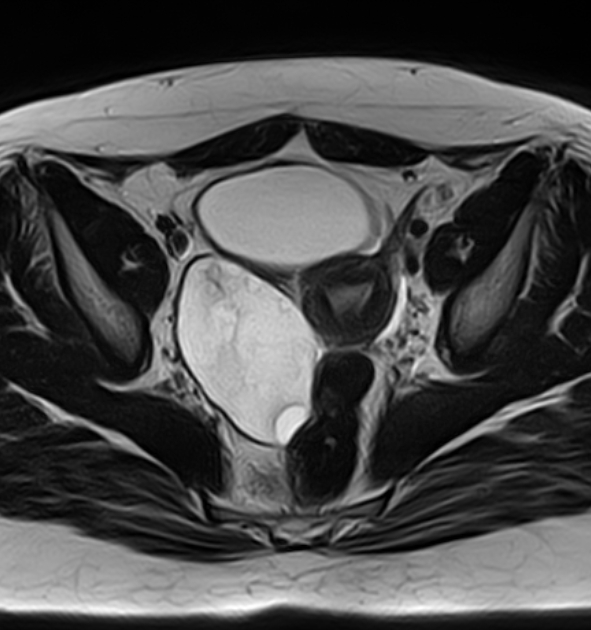
MRI
Sometimes the diagnosis of ovarian torsion is missed and the patient may be referred for MRI to evaluate a mass. The delay makes infarction more likely 4.
T1: may show a thin rim of high signal intensity (methemoglobin) 29
T2: may have low signal due to interstitial hemorrhage 30
T1 C+ (Gd): reduced or no contrast enhancement 26,27
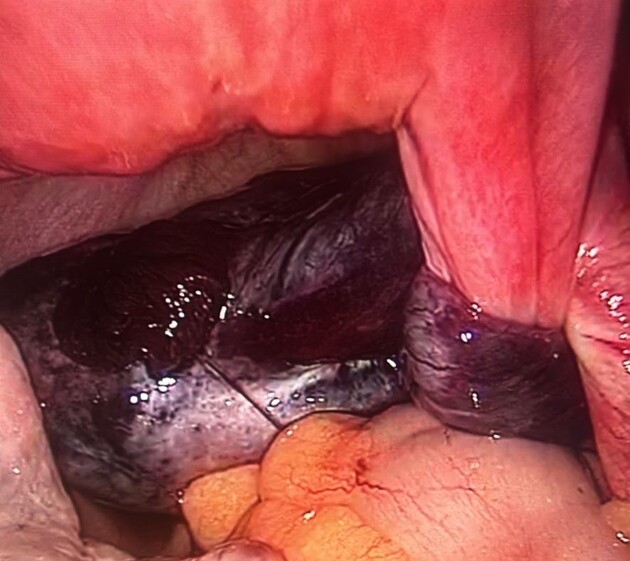
Treatment and prognosis
Urgent surgery is indicated to prevent ovarian necrosis. The appearances at surgery can be misleading; a non-friable blue/black ovary may regain function over time. Oophoropexy will prevent recurrence.
A salpingo-oophorectomy is appropriate for postmenopausal women or suspected malignancy.
A necrotic ovary may involute, bleed or become infected leading to abscess formation or peritonitis.
Long-term complications include pelvic pain, adhesions and tubal infertility.
Differential diagnosis
ectopic pregnancy: positive beta HCG
ruptured ovarian cyst: abrupt (midcycle) pain and free fluid / hemoperitoneum
pelvic inflammatory disease: indolent disease course, signs of inflammation
massive ovarian edema due to malignant lymphatic obstruction
ovarian mass
degenerating pedunculated leiomyoma
appendicitis: inflamed pelvic appendix may be seen on ultrasound
Practical points
the imaging diagnosis is often missed
edematous swelling of the ovary is the hallmark of torsion
the affected ovary may be too high or too low, or may be anterior or posterior to the uterus
the uterus may be tilted
whirlpool sign is specific, but difficult to identify on CT
absence of ovarian Doppler flow is highly specific for torsion, but normal Doppler flow does not exclude torsion
the presence of blood flow is a marker for viability
an ovarian mass presenting with severe pain is suspicious for torsion; masses are rarely painful otherwise
ovarian masses cause thinning of the ovarian tissue; smooth or eccentric thickening of ovarian tissue around a mass is suspicious for torsion































 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.