Pericarditis is defined as inflammation of the pericardium. It is normally found in association with cardiac, thoracic or wider systemic pathology and it is unusual to manifest on its own.
On this page:
Epidemiology
Pericarditis is the most common pericardial disease worldwide and accounts for about 0.1-0.2% of all hospital admissions and about 5% of chest pain admissions to the emergency department 1-4.
Associations
Diagnosis
The diagnosis of pericarditis is based on clinical criteria and supplemental imaging information 1.
Diagnostic criteria
According to the 2015 European Society of Cardiology (ESC) Guidelines for the diagnosis and management of pericardial diseases the diagnosis can be made if ≥2 of the following four criteria are met 1:
pericarditic chest pain
pericardial rubs
new widespread ST elevation and/or PR depression (ECG)
new or worsening pericardial effusion
Supporting findings include the following:
imaging findings on cardiac CT or cardiac MRI suggesting pericardial inflammation
Clinical presentation
Classically, patients present with abrupt, pleuritic, positional left precordial chest pain after a viral prodrome. The pain is relieved in the sitting position when leaning forward and exacerbated when supine. Tuberculous pericarditis may present with constitutional symptoms, including fever, night sweats, anorexia, and weight loss. The physical exam may demonstrate:
-
a pericardial friction rub
classically triphasic, two components in diastole and one in systole
may be transient
-
signs of tamponade
classically Beck triad, with jugular venous distension, hypotension, and muffled heart sounds
ECG
-
diffuse ST-segment elevation (STE)
with upward concavity
the STE in lead II > lead III
absence of reciprocal changes or Q waves
-
lead aVR demonstrates ST-segment depression
this lead also may demonstrate PR segment elevation
-
diffuse PR segment depression
excluding the aforementioned (lead aVR)
later, T-wave inversions may develop
Pathology
Aetiology
Aetiologies can be divided into infectious (viral, bacterial, fungal and parasitic) and non-infectious causes (autoimmune, neoplastic and metabolic), with infections accounting for two-thirds of cases and non-infectious causes for the remaining third 1,5.
Classification
Pericarditis can be divided into subtypes according to morphology:
Acute forms
Established forms
Radiographic features
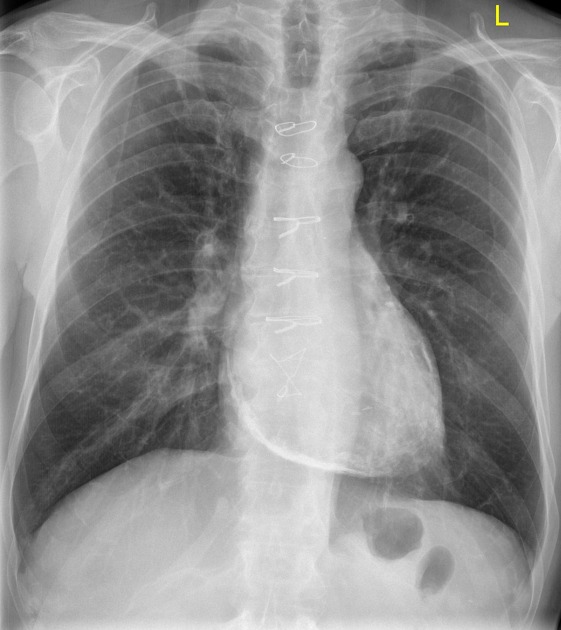
Plain radiograph
There may be an increased cardiothoracic ratio (CTR) with a globular or 'flask-shaped' outline if there is co-existing pericardial effusion. Manifestations of cardiogenic pulmonary oedema may also be present.
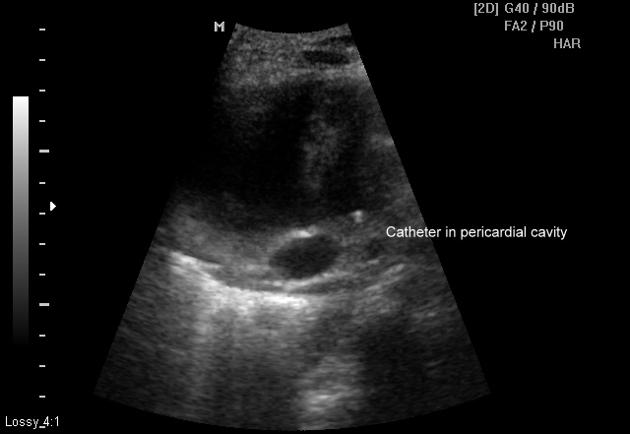
Ultrasound
Echocardiography is recommended when the pericardial disease is suspected and may demonstrate 11:
-
indication for hospitalisation when new and large
cardiac tamponade
elevated filling pressures
Patients who have a preserved ejection fraction but symptomatic heart failure may (with a suggestive clinical history) be examined for occult constrictive pericarditis, features of which include:
-
mitral/tricuspid inflow pulsus paradoxus
in the absence of an effusion
-
annulus paradoxus
elevated filling pressures with a preserved mitral septal annular velocity (septal e')
-
annulus reversus
tissue Doppler of the mitral annuli reveals a septal e' > lateral e'
the lateral e' is normally always higher than the septal e'
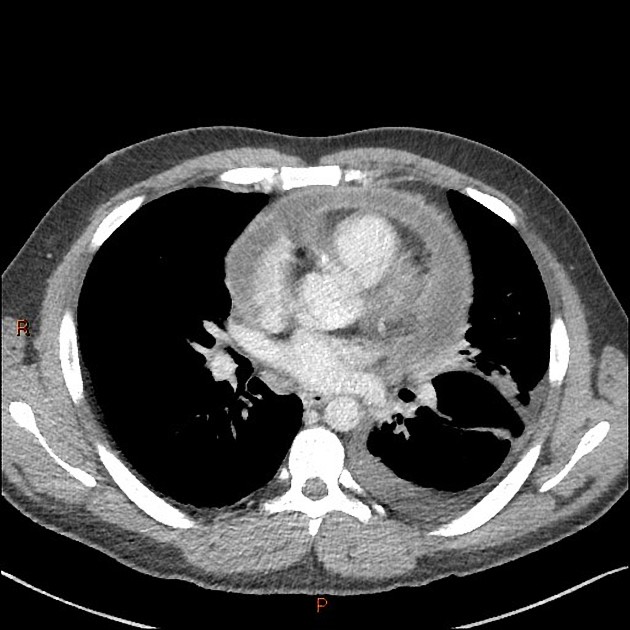
CT
At contrast-enhanced CT, enhancement of the thickened pericardium generally indicates inflammation 1.
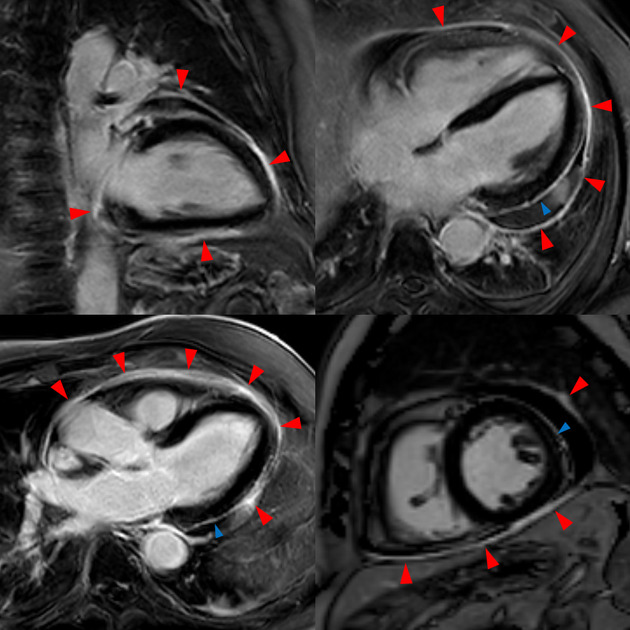
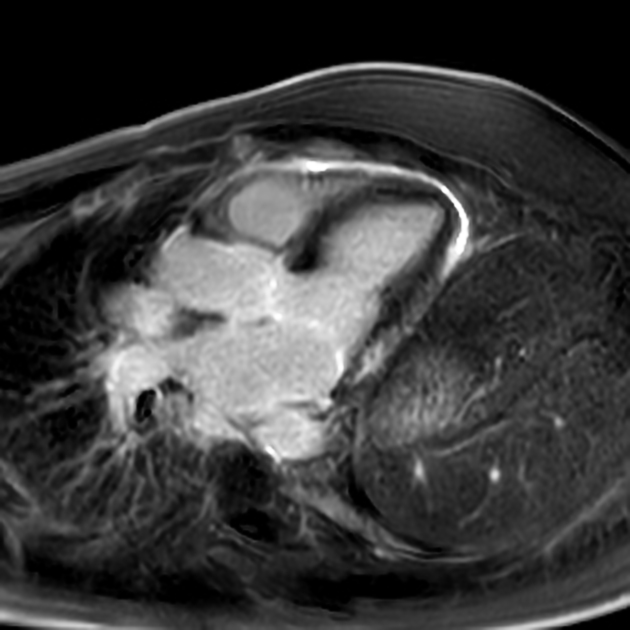
MRI
Usually, GRE cine, T1, T2 black-blood/STIR and IR GRE sequences are performed. In the setting of suspected pericardial constriction, real-time cine sequences should be acquired 6,7. The presence of an arrhythmia may induce artifacts. For specific features please refer to subtype articles.
The normal pericardial thickness is considered 2 mm while a thickness of over 4 mm suggests a pericarditis 8,9.
Oedema of the visceral and parietal pericardium, depicted in T2 black-blood/STIR images, and enhancement usually assessed with late gadolinium enhancement (LGE) images are additional specific MRI features 6,7,10.
In addition, cardiac MRI has the ability to assess the myocardium regarding concomitant myocarditis and viability in a post-myocardial infarction setting or to detect myocardial infarction, if previously unknown.
Nuclear medicine
PET
Focal FDG uptake may be demonstrated in some cases.








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.