A perilymphatic fistula (also known as a perilymph fistula or labyrinthine fistula) is a pathologic communication between the fluid-filled space of the inner ear and the air-filled space of the middle ear, most commonly occurring at either the round or oval window.
On this page:
Clinical presentation
Although perilymphatic fistulas may be spontaneous, a definite diagnosis is characterized by acute onset preceded by a traumatic event (barotrauma or direct trauma) 1.
Symptoms of perilymphatic fistula include the following:
-
audiological symptoms
tinnitus
-
vestibular symptoms
vertigo, dizziness, or disequilibrium
nausea
ear fullness
On exam, a positive perilymph fistula test consists of examiner pressure on the tragus and external auditory canal that induces nystagmus 2.
Pathology
A perilymphatic fistula can be due traumatic, iatrogenic, or intrinsic processes that affect the otic capsule, oval window, or round window. Examples include the following 1,2:
blunt trauma (otic capsule-violating temporal bone fracture)
penetrating trauma (ear pick or cotton swab)
barotrauma (explosion, pinched nose Valsalva maneuver, altitude/depth change)
surgery (stapedotomy, stapedectomy, cochleostomy, cochlear implant)
middle and inner ear diseases (chronic otitis media with cholesteatoma causing lateral semicircular canal dehiscence)
idiopathic
Radiographic features
CT
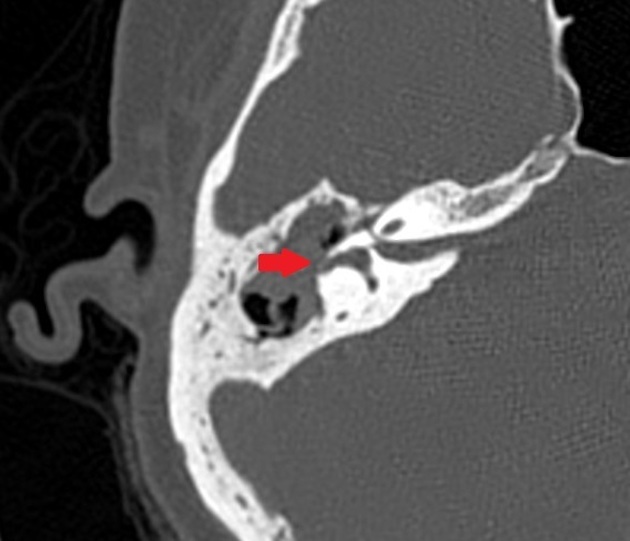
The first-line imaging test for suspected perilymphatic fistula is a dedicated, high-resolution temporal bone CT, which can show the following signs 1,3:
pneumolabyrinth (air in the vestibule, semicircular canals, and/or cochlea): specific but not sensitive
fluid in the oval or round window niches: sensitive but not specific
bony injuries (disorientation of the stapes footplate relative to the oval window, otic capsule-violating fracture, dehiscence of lateral semicircular canal, etc.)
MRI
may demonstrate fluid-filling in the round window (especially if >2/3 of the round window niche) or in the oval window niches (considered most common sign 3
may demonstrate a round window sign, defined as a nodular FLAIR high signal in the round window and the presence of associated saccular hydrops 4
Treatment and prognosis
Conservative management may be considered in idiopathic cases, with counseling to avoid activities that increase intracranial or inner ear pressure 1. Surgical management is indicated if conservative management fails and/or a clear cause is identified. Techniques include blood patch and grafting the injured window (such as with fat, fascia, perichondrium, or gelatin sponge) 1.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.