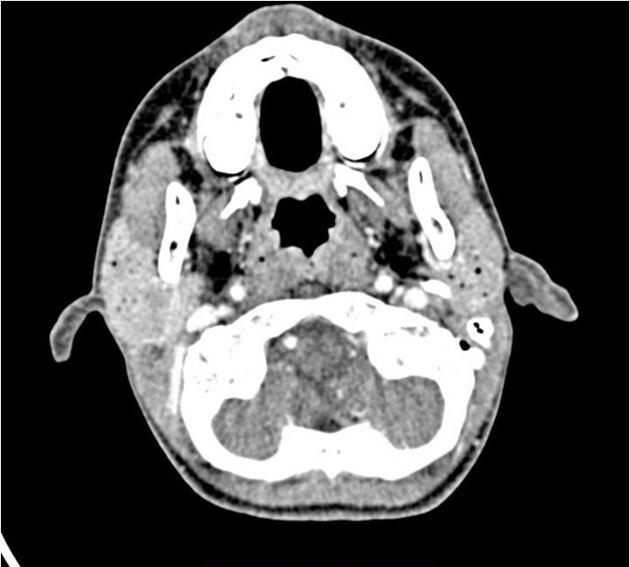
Pneumoparotid refers to gas in the parotid gland and can cause unilateral or bilateral parotid swelling. In severe cases, it can be associated with subcutaneous emphysema.
On this page:
Terminology
Both pneumatocele glandulae parotis and parotid emphysema have also been used to describe the presence of gas in the parotid.
Pneumoparotitis is used when pneumoparotid is complicated by a secondary infection, usually by oral bacterial commensals 5,6. The term pneumosialadenitis has also been used but is less precise as it could also be used for an inflamed submandibular gland with internal gas.
Epidemiology
Pneumoparotid is rare, with only 54 cases reported in the global literature from 1987-2020 4. In this cohort, 72% of cases were male.
Pneumoparotid can be seen in any profession or recreation that increases oral positive pressure, causing air to reflux up the parotid ducts into the parotid gland.
Risk factors
Activities causing elevated intraoral air pressure:
brass/woodwind players
glassblowers
underwater divers
blowing up inflatable pool toys orally
Other proposed risk factors include 4:
hypotonic buccinator muscles
transient Stensen duct obstruction due to mucus
Clinical presentation
Typically, in a pure pneumoparotid, the parotid gland swelling is mild and painless (occasionally mild achiness), without a fever 4. Occasionally crepitus can be felt in the gland 5.
Gas within the submandibular gland, a.k.a. "pneumosialodenitis of the submandibular gland", has also been described but seems to be much rarer 7.
Complications
subcutaneous emphysema: up to 20% cases 4
pneumomediastinum (rare)
Pathology
Etiology
Increased oral positive air pressure can cause retrograde reflux of air into the main parotid duct, and into the parotid gland. Causes include:
-
occupational/recreational
brass/woodwind players
glass blowers
underwater divers
-
pulmonary diseases associated with recurrent coughing 5
-
iatrogenic
positive-pressure ventilation
spirometry 4
dental procedures using air-powered equipment
-
other
-
self-induced parotid insufflation/Valsalva maneuver
equalising middle ear pressures on aircraft
suppressing chronic cough
psychiatric disorders 2
-
Rarely gas in the parotid is not due to elevated intraoral pressures but air/gas introduced by other causes, e.g. FNA, trauma
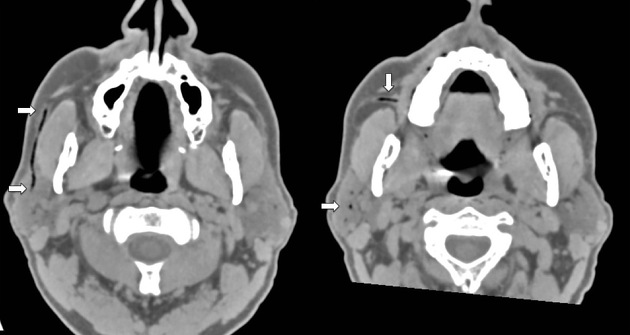
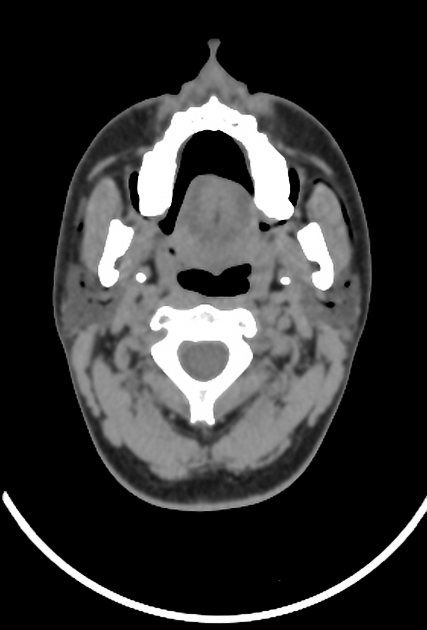
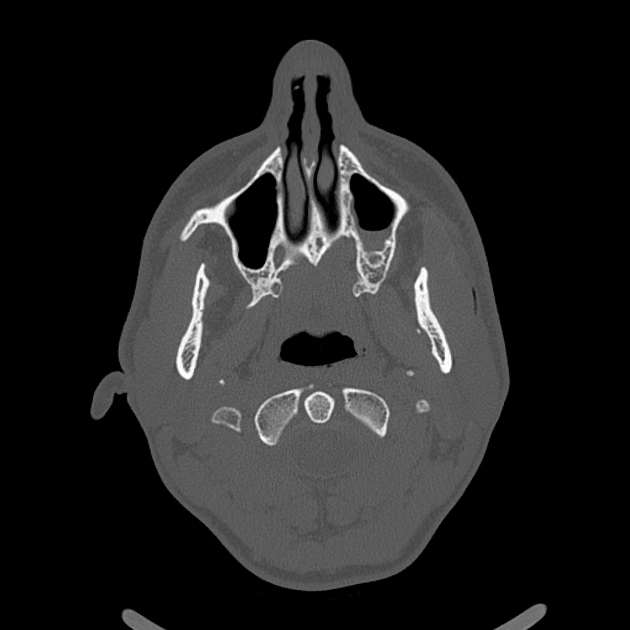
Radiographic features
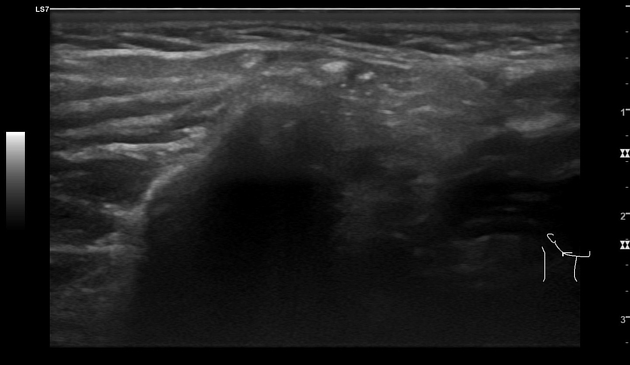
Gas can be shown within the parotid on x-ray, ultrasound, CT and MRI, with CT being the most sensitive 2-5. On ultrasound stones and gas foci are both reflective, but stones demonstrate posterior acoustic shadowing, whilst ring-down/reverberation artifacts occur distal to gas bubbles.
Treatment and prognosis
Many cases are self-limiting and treatment is conservative.
antibiotics: prophylaxis against superadded infection
analgesia
-
supportive expulsion of gas from parotid
gland massage, external compresses,
sialogogues
surgery is reserved for recurrent/severe cases and is rarely performed
Complications
infective parotitis: due to recurrent pneumoparotid
Differential diagnosis
Clinically, the presentation needs to be differentiated from other causes of swelling of the parotid gland. However once imaging has shown the gas within the parotid gland, then no differential needs to entertained.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.