Pulsatility index (ultrasound)
Citation, DOI, disclosures and article data
At the time the article was created David Carroll had no recorded disclosures.
View David Carroll's current disclosuresAt the time the article was last revised Daniel J Bell had no recorded disclosures.
View Daniel J Bell's current disclosures- Pulsatility index (PI)
- Gosling index
- Gosling pulsatility index
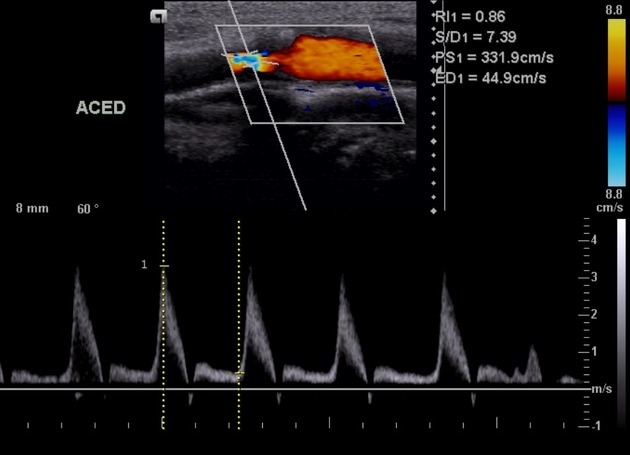
The pulsatility index (PI) (also known as the Gosling index) is a calculated flow parameter in ultrasound, derived from the maximum, minimum, and mean Doppler frequency shifts during a defined cardiac cycle. Along with the resistive index (RI), it is typically used to assess the resistance in a pulsatile vascular system.
On this page:
Terminology
Pulsatility is an intrinsic property of the cardiovascular system, governed by the resistance differential across the arteriolar bed, which allows the potential energy stored in the elastic, proximal arteries to propagate throughout the microcirculation at a mean pressure consistent with adequate perfusion.
When evaluated as a derived flow parameter using pulsed wave Doppler, it is calculated by one of the following equations:
PI = (vmax - vmin) / (vmean)
PI = (peak systolic velocity - minimal diastolic velocity) / (mean velocity)
The operator typically recognises and demarcates maximum (vmax) and minimum (vmin) velocities, while the mean velocity (vmean) is calculated by the ultrasound machine.
ADVERTISEMENT: Supporters see fewer/no ads
Clinical use
Because the calculation of these flow parameters is based on the same Doppler spectrum, possible instrument-dependent errors, or an inappropriate angle of insonation by the user, are mitigated somewhat 1.
Clinical scenarios in which a pulsatility index are calculated include:
- malignant ovarian lesions
- transcranial Doppler
- carotid artery evaluation for stenosis
- umbilical vein Doppler
- fetal middle cerebral artery Doppler - fetal middle cerebral artery pulsatility index
- umbilical arterial pulsatility index
History and etymology
The pulsatility index was described in a 1974 paper by Raymond Gosling (1926-2015) 4, a British biophysicist. He is more famously remembered as working under the team led by Rosalind Franklin when x-ray crystallography was used to investigate DNA. From this work James Watson and Francis Crick inferred the structure of DNA for which they shared the Nobel prize 2,3.
References
- 1. Boote EJ. AAPM/RSNA physics tutorial for residents: topics in US: Doppler US techniques: concepts of blood flow detection and flow dynamics. (2003) Radiographics : a review publication of the Radiological Society of North America, Inc. 23 (5): 1315-27. doi:10.1148/rg.235035080 - Pubmed
- 2. Michel E, Zernikow B. Gosling's Doppler pulsatility index revisited. (1998) Ultrasound in medicine & biology. 24 (4): 597-9. doi:10.1016/s0301-5629(98)00024-6 - Pubmed
- 3. Gosling RG, King DH. Arterial assessment by Doppler-shift ultrasound. (1974) Proceedings of the Royal Society of Medicine. 67 (6 Pt 1): 447-9. Pubmed
- 4. A. M. Glazer. Crystallography. (2016) ISBN: 9780198717591
Incoming Links
- Cerebroplacental ratio
- Abnormal ductus venosus waveforms
- Fetal middle cerebral artery pulsatility index
- Ovarian serous cystadenocarcinoma
- Uteroplacental blood flow assessment
- Medical abbreviations and acronyms (P)
- Resistive index (vascular ultrasound)
- Umbilical arterial pulsatility index
- Pre-eclampsia
- Raised intracranial pressure
- Transcranial Doppler sonography (ultrasound)
- Common hepatic artery
- Malignant ovarian lesions (sonographic features)
Related articles: Imaging technology
- imaging technology
- imaging physics
- imaging in practice
-
x-rays
- x-ray physics
- x-ray in practice
- x-ray production
- x-ray tube
- filters
- automatic exposure control (AEC)
- beam collimators
- grids
- air gap technique
- cassette
- intensifying screen
- x-ray film
- image intensifier
- digital radiography
- digital image
- mammography
- x-ray artifacts
- radiation units
- radiation safety
- radiation detectors
- fluoroscopy
-
computed tomography (CT)
- CT physics
- CT in practice
- CT technology
- CT image reconstruction
- CT image quality
- CT dose
-
CT contrast media
-
iodinated contrast media
- agents
- water soluble
- water insoluble
- vicarious contrast material excretion
- iodinated contrast media adverse reactions
- agents
- non-iodinated contrast media
-
iodinated contrast media
-
CT artifacts
- patient-based artifacts
- physics-based artifacts
- hardware-based artifacts
- ring artifact
- tube arcing
- out of field artifact
- air bubble artifact
- helical and multichannel artifacts
- CT safety
- history of CT
-
MRI
- MRI physics
- MRI in practice
- MRI hardware
- signal processing
-
MRI pulse sequences (basics | abbreviations | parameters)
- T1 weighted image
- T2 weighted image
- proton density weighted image
- chemical exchange saturation transfer
- CSF flow studies
- diffusion weighted imaging (DWI)
- echo-planar pulse sequences
- fat-suppressed imaging sequences
- gradient echo sequences
- inversion recovery sequences
- metal artifact reduction sequence (MARS)
-
perfusion-weighted imaging
- techniques
- derived values
- saturation recovery sequences
- spin echo sequences
- spiral pulse sequences
- susceptibility-weighted imaging (SWI)
- T1 rho
- MR angiography (and venography)
-
MR spectroscopy (MRS)
- 2-hydroxyglutarate peak: resonates at 2.25 ppm
- alanine peak: resonates at 1.48 ppm
- choline peak: resonates at 3.2 ppm
- citrate peak: resonates at 2.6 ppm
- creatine peak: resonates at 3.0 ppm
- functional MRI (fMRI)
- gamma-aminobutyric acid (GABA) peak: resonates at 2.2-2.4 ppm
- glutamine-glutamate peak: resonates at 2.2-2.4 ppm
- Hunter's angle
- lactate peak: resonates at 1.3 ppm
- lipids peak: resonates at 1.3 ppm
- myoinositol peak: resonates at 3.5 ppm
- MR fingerprinting
- N-acetylaspartate (NAA) peak: resonates at 2.0 ppm
- propylene glycol peak: resonates at 1.13 ppm
-
MRI artifacts
- MRI hardware and room shielding
- MRI software
- patient and physiologic motion
- tissue heterogeneity and foreign bodies
- Fourier transform and Nyquist sampling theorem
- MRI contrast agents
- MRI safety
-
ultrasound
- ultrasound physics
-
transducers
- linear array
- convex array
- phased array
- frame averaging (frame persistence)
- ultrasound image resolution
- imaging modes and display
- pulse-echo imaging
- real-time imaging
-
Doppler imaging
- Doppler effect
- colour Doppler
- power Doppler
- B flow
- colour box
- Doppler angle
- pulse repetition frequency and scale
- wall filter
- colour write priority
- packet size (dwell time)
- peak systolic velocity
- end-diastolic velocity
- resistive index
- pulsatility index
- Reynolds number
- panoramic imaging
- compound imaging
- harmonic imaging
- elastography
- scanning modes
- 2D ultrasound
- 3D ultrasound
- 4D ultrasound
- M-mode
-
ultrasound artifacts
- acoustic shadowing
- acoustic enhancement
- beam width artifact
- reverberation artifact
- ring down artifact
- mirror image artifact
- side lobe artifact
- speckle artifact
- speed displacement artifact
- refraction artifact
- multipath artifact
- anisotropy
- electrical interference artifact
- hardware-related artifacts
- Doppler artifacts
- aliasing
- tissue vibration
- spectral broadening
- blooming
- motion (flash) artifact
- twinkling artifact
- acoustic streaming
- biological effects of ultrasound
- history of ultrasound
-
nuclear medicine
- nuclear medicine physics
- detectors
- tissue to background ratio
-
radiopharmaceuticals
- fundamentals of radiopharmaceuticals
- radiopharmaceutical labelling
- radiopharmaceutical production
- nuclear reactor produced radionuclides
- cyclotron produced radionuclides
- radiation detection
- dosimetry
- specific agents
- carbon-11
- chromium-51
- fluorine agents
- gallium agents
- Ga-67 citrate
- Ga-68
- iodine agents
-
I-123
- I-123 iodide
- I-123 ioflupane (DaTSCAN)
- I-123 ortho-iodohippurate
- I-131
-
MIBG scans
- I-123 MIBG
- I-131 MIBG
-
I-123
- indium agents
- In-111 Octreoscan
- In-111 OncoScint
- In-111 Prostascint
- In-111 oxine labelled WBC
- krypton-81m
- nitrogen-13
- oxygen-15
- phosphorus-32
- selenium-75
-
technetium agents
- Tc-99m DMSA
- Tc-99m DTPA
- Tc-99m DTPA aerosol
- Tc-99m HMPAO
- Tc-99m HMPAO labelled WBC
- Tc-99m MAA
- Tc-99m MAG3
- Tc-99m MDP
- Tc-99m mercaptoacetyltriglycine
- Tc-99m pertechnetate
- Tc-99m labelled RBC
- Tc-99m sestamibi
- Tc-99m sulfur colloid
- Tc-99m sulfur colloid (oral)
- thallium-201 chloride
- xenon agents
- in vivo therapeutic agents
- pharmaceuticals used in nuclear medicine
-
emerging methods in medical imaging
- radiography
- phase-contrast imaging
- CT
- deep-learning reconstruction
- photon counting CT
- virtual non-contrast imaging
- ultrasound
- magnetomotive ultrasound (MMUS)
- superb microvascular imaging
- ultrafast Doppler imaging
- ultrasound localisation microscopy
- MRI
- nuclear medicine
- total body PET system
- immuno-PET
- miscellaneous
- radiography




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.