Septic arthritis can cause rapid chondrolysis and destructive arthropathy. Intra-articular infection usually manifests with severe pain and decreased range of motion. Prompt treatment can avoid permanent damage to the joint which may result in chronic deformity, mechanical arthritis and even death 7.
On this page:
Epidemiology
Septic arthritis should be considered in any patient with acute monoarthritis.
Risk factors
Risk factors for septic arthritis include:
bacteraemia
advanced age
sexually active
immunocompromised state
intra-articular injections
prosthetic joints
Clinical presentation
The diagnosis of joint sepsis is often considered straightforward. Patients often present with a painful joint, fever and purulent synovial fluid.
Pathology
Aetiology
In the absence of trauma or recent instrumentation of the joint, septic arthritis is usually secondary to haematogenous seeding. Staphylococcus aureus is the most commonly isolated agent 6 and Streptococci spp. are common; both these organisms can cause rapid joint destruction. Other pathogens include Pseudomonas, Escherichia coli, and Serratus 10.
Haemophilus influenzae was once a common causative agent for septic arthritis in children under the age of 2 but has significantly reduced in incidence due to vaccination 8,9. Gonococcal bacteraemia 9 is more common in sexually active individuals and responds well to appropriate antibiotics, usually with no sequelae.
Location
Large joints with abundant blood supply to the metaphyses are most prone to bacterial infection, with the most commonly affected joints theoretically being the shoulder, hip, and knee.
In intravenous drug users, the sternoclavicular and sacroiliac joints are more frequently affected.
Classification
The Hunka classification is used to grade the anatomical deformity following septic arthritis in a paediatric hip.
Radiographic features
Imaging generally plays an adjunct role to arthrocentesis in the diagnosis of joint sepsis. If synovial fluid cannot be retrieved, however, radiologic studies become of the utmost importance.
Plain radiograph
may be normal in the very early stage of the disease
joint effusion may be seen
juxta-articular osteoporosis due to hyperaemia
narrowing of the joint space due to cartilage destruction in the acute phase
destruction of the subchondral bone on both sides of a joint
if left untreated, reactive juxta-articular sclerosis and, in severe cases, ankylosis will develop
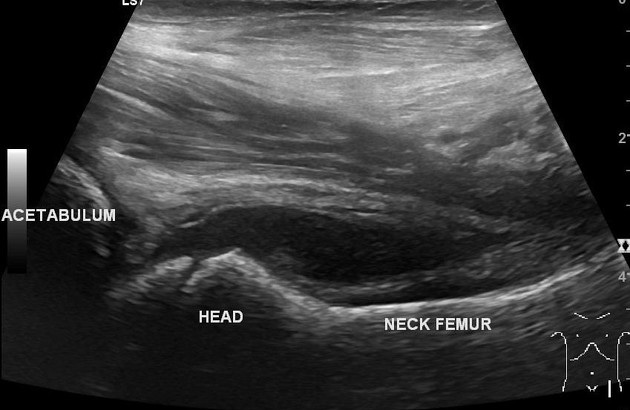
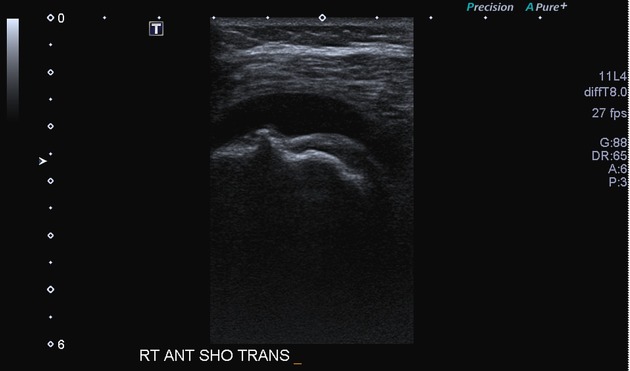
Ultrasound
useful in superficial joints and in children
-
shows joint effusion
echogenic debris may be present
colour Doppler may show increased perisynovial vascularity
can be used to guide joint aspiration
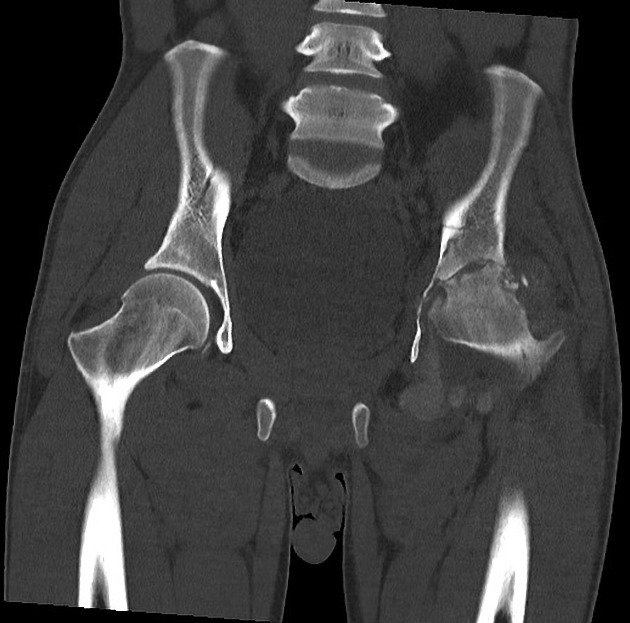
CT
CT features of septic arthritis are similar to those spotted on radiographs
a fat-fluid level can be a specific sign in the absence of trauma
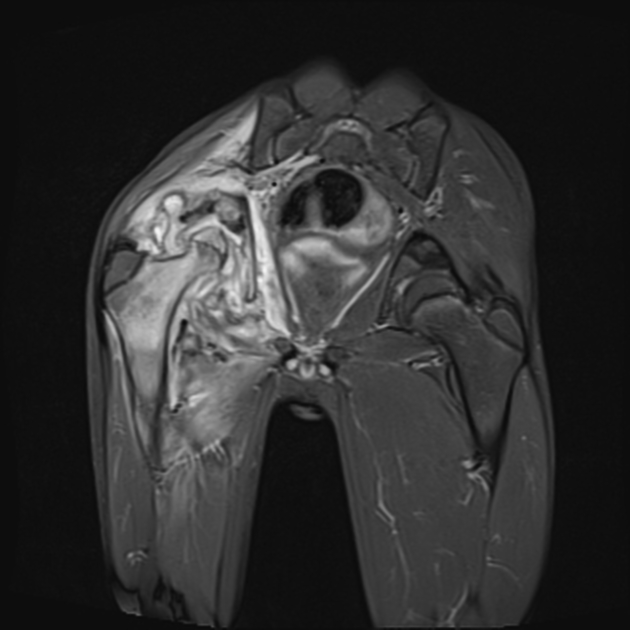
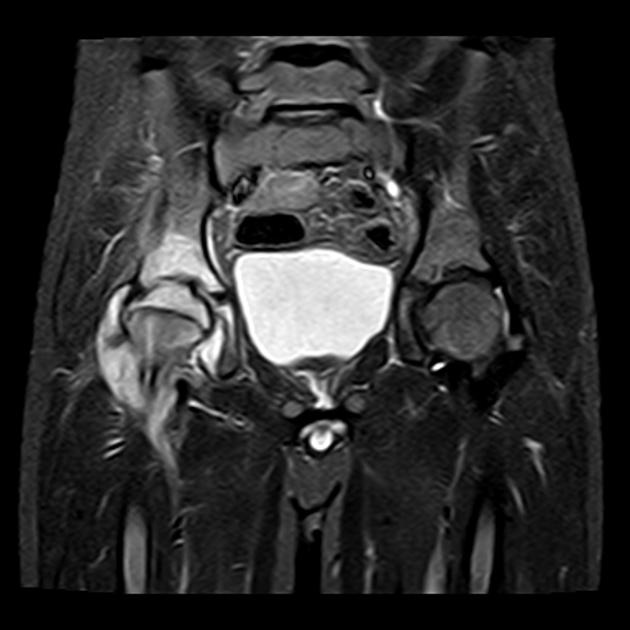
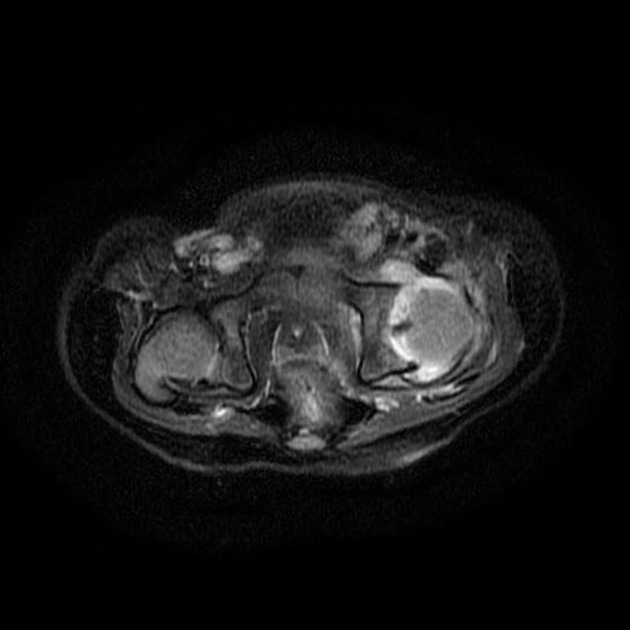
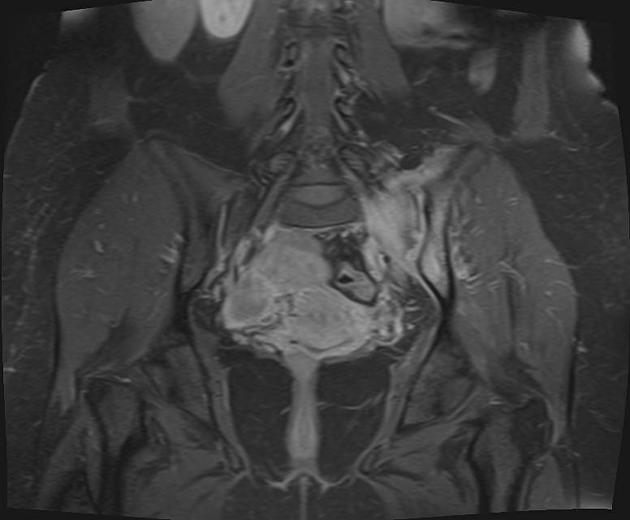
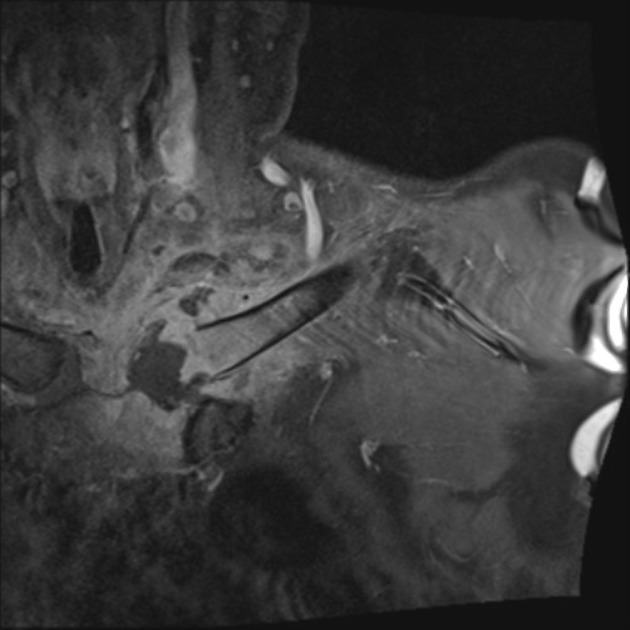
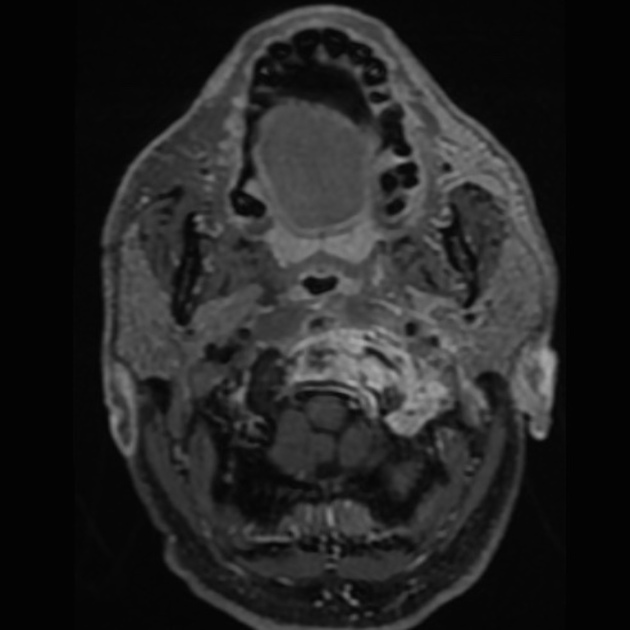
MRI
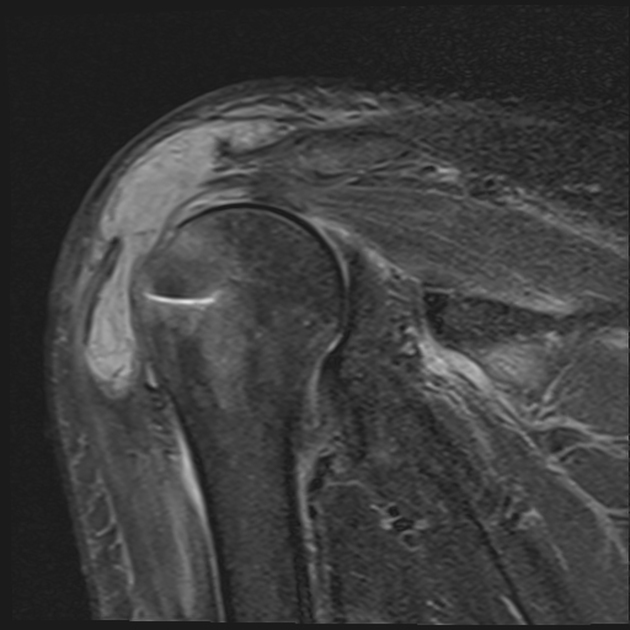
MRI is sensitive and more specific for early cartilaginous damage with joint effusion being characterisation 10.
T1: low signal within the subchondral bone
T2: thin rim of subchondral oedema; pericapsular oedema 10
T1 C+ (Gd): synovial enhancement reflecting synovitis; pericapsular enhancement 10
Treatment and prognosis
The treatment principle for septic arthritis is prompt drainage of purulent fluid and appropriate antibiotics 7.
If the patient is hemodynamically stable then attempts should be made to obtain a sample of joint fluid for microscopy and culture prior to starting treatment with antibiotics. This will allow focussed treatment of the infection 4.
With smaller joints needle drainage or aspiration to decompress the joint followed by antibiotics may be adequate. For larger joints or persistent infection, surgical debridement and washout will be required 4.
If unrecognised and left untreated, septic arthritis can result in irreversible joint damage within 48 hours of the onset of infection due to the proteolytic enzymes of the white blood cells that flood the infected synovial space. Osteonecrosis is also an important sequela of septic arthritis due to effusion and an increase in intra-articular pressure which compromises blood circulation.
Conversely, approximately 90% of patients with septic arthritis will recover with appropriate antibiotic treatment. Therefore, timely diagnosis and treatment are critical.
Practical points
osteomyelitis should be suspected if bone marrow oedema extends in the medullary space in the setting of suspected or proven septic arthritis 10














 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.