A skeletal survey in non-accidental injury is a defined set of images that are obtained to assess the majority of the bones in the child. Referral for a skeletal survey in this context will usually come from a member of the child protection team, and there should be a thorough discussion about their concerns before the study being performed. In most cases, this study should only be performed in an institution where the radiographers have appropriate training and where there is access to pediatric radiology opinion and review during the study.
On this page:
United Kingdom
In the UK, a skeletal survey is composed of 1:
-
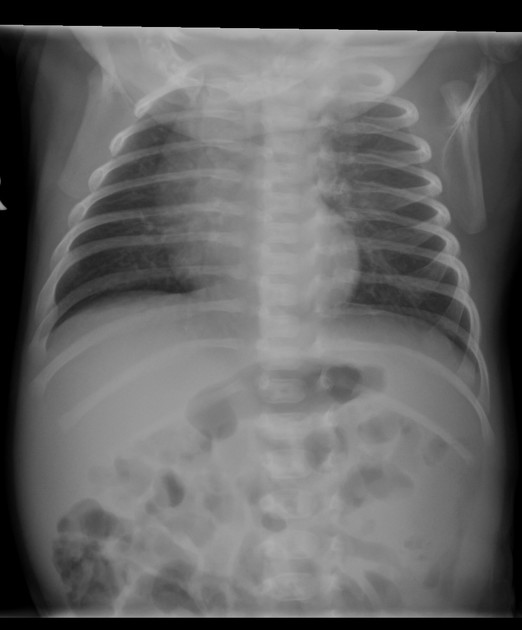
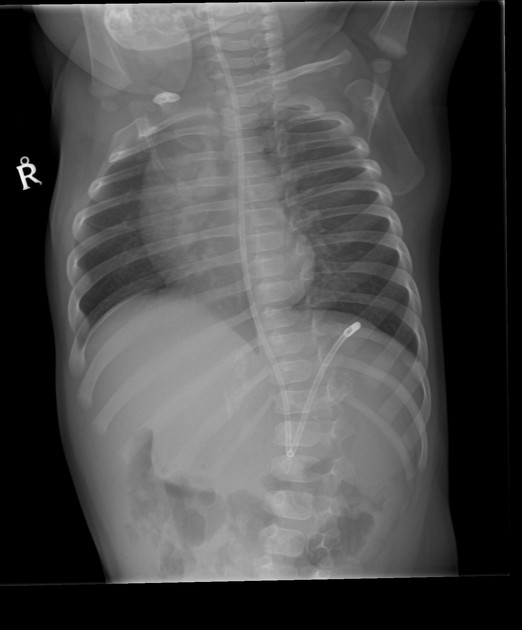
torso
ribs (oblique) (left and right)
whole lateral spine
-
upper limbs (each)
-
lower limbs (each)
AP femur
AP tib/fib
The humerus and forearm may be imaged as a single AP if the quality is appropriate. This is also true of the femur and tib/fib.
In all under one year old and in all children where there is neurology or encephalopathy, a CT head should be performed. Where a CT is not performed, skull radiographs should be performed.
Australia and New Zealand
In Australia and New Zealand, the primary skeletal survey is comprised of 2:
-
head, chest, spine and pelvis
AP and lateral skull (if CT has not been performed)
AP chest (including the shoulders)
ribs (oblique) (left and right)
AP abdomen and pelvis
whole lateral spine
-
upper limbs (each)
-
AP arm (centered at the elbow)
-
if the child is too large
AP humerus, including the shoulder and elbow
AP forearm, including the wrist and elbow
-
lateral elbow
lateral wrist
PA hand and wrist
-
-
lower limbs (each)
-
AP lower limb hip to ankle
-
if the child is too large
AP femur
AP tibia and fibula
-
lateral knee
lateral ankle
AP knee
DP foot
-
Practical points
a single radiograph of the entire patient, i.e. a 'babygram', is not a recommended nor appropriate exam for the assessment of suspected non-accidental injuries 1,2
skeletal surveys are technically and emotionally demanding, they require specially trained radiographers with a clear understanding of the process
often centers require a minimal of two radiographers with specialized training in the room at all times, with the use of anatomical markers (rather than digital) 1
quality images, free from motion artifact, are important. Use of appropriate immobilization techniques should be considered, including the use of adults to assist holding the patient; if this is done, all parties involved must be documented




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.