Meningiomas arising from the coverings of the spinal cord are one of the two most common intradural extramedullary spinal tumours, representing 25-30% of all such tumours 2.
This article specifically relates to spinal meningiomas. For a discussion on intracranial meningiomas and a general discussion of the pathology refer to the main article: meningioma.
On this page:
Epidemiology
Spinal meningiomas represent a minority of all meningiomas (approximately 12%) 5. They have a peak incidence in the sixth through eighth decades 8.
Spinal meningiomas have a strong sex predilection in adults, stronger than that seen with intracranial meningiomas, with females accounting for 75-90% of cases 8. In children, there does not appear to be a sex predilection.
Risk factors
The best recognised environmental risk factor is exposure to high dose ionising radiation, especially in childhood 10. Prior trauma is another risk factor 10.
Associations
There is an increased incidence of spinal meningiomas in patients with neurofibromatosis type 2 (NF2). In fact, in the paediatric population, meningiomas uncommonly occur outside of the setting of NF2.
Clinical presentation
Despite usually being small, due to the confines of the spinal canal, spinal meningiomas can result in significant neurologic dysfunction. The majority of patients present with motor deficits as a result of compression of the spinal cord. Less common presentations include sensory deficits, pain and sphincter dysfunction.
Pathology
Most spinal meningiomas are benign, with 70-90% being classified as WHO grade I lesions 8. Less common are tumours with more aggressive features consistent with WHO grade II (5-25%) or grade III (1-5%).
There are many histomorphometric variants of meningioma recognised in the WHO classification. The most common spinal meningioma histology is WHO grade I meningothelial meningioma (80%) 9. WHO grade II clear cell meningiomas have a predilection for the spine and are believed to originate from the denticulate ligaments 6,7.
For a discussion of the pathology of meningiomas, refer to the general meningioma article.
Radiographic features
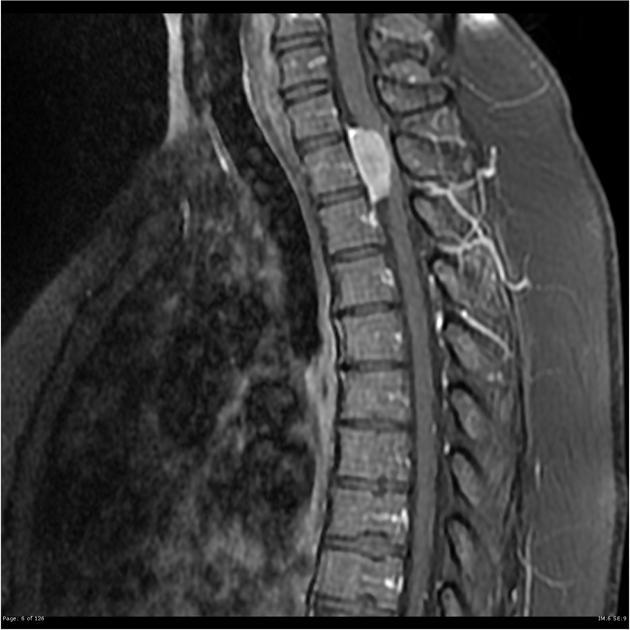
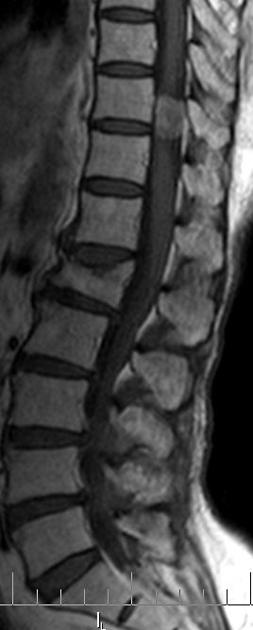
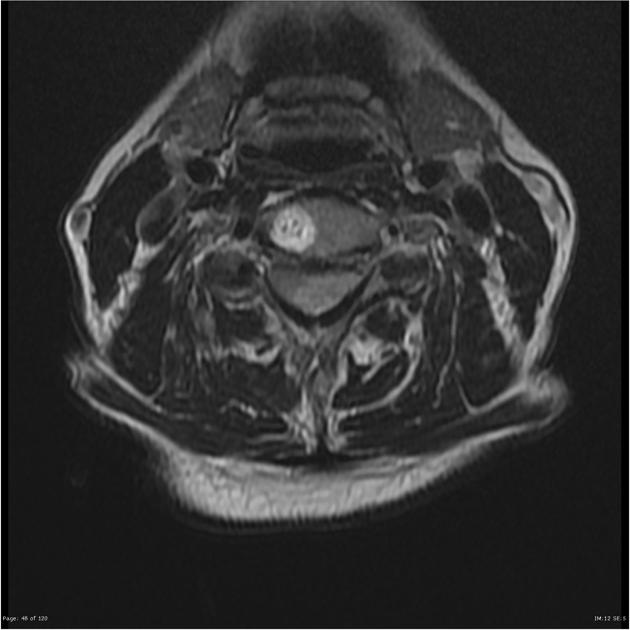
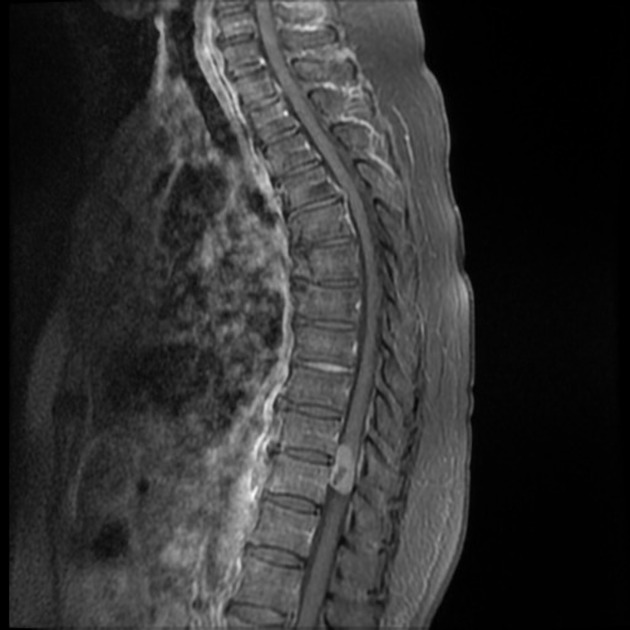
The vast majority (90%) of spinal meningiomas are intradural extramedullary in location. Occasionally (5%), purely extradural tumours are found. The remainder (5%) have both intradural and extradural components taking on a dumbbell appearance 2.
Spinal meningiomas are not distributed evenly along the canal 2:
cervical spine: 15%
thoracic spine: 80%
lumbosacral spine: 5%
Meningiomas are most often located lateral to the spinal cord (60-70%) 11,12. Those in the cervical spine are more likely to be located anteriorly compared to those in the thoracic spine 6.
Most meningiomas are solitary lesions (98%). Multiple meningiomas are most often associated with NF2 6.
Plain radiograph
usually normal
rarely bone erosion or calcification
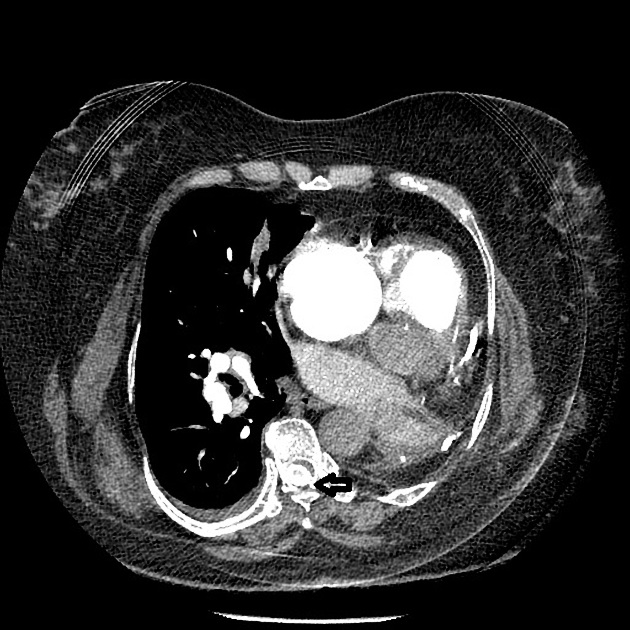
CT
isodense or moderately hyperdense mass
hyperostosis may be seen but is not as common as in the intracranial forms
calcification may be present but are uncommon (5%) 8
CT myelography
arachnoid isolation sign: intradural tumour separated from spinal cord by contrast in subarachnoid space 13
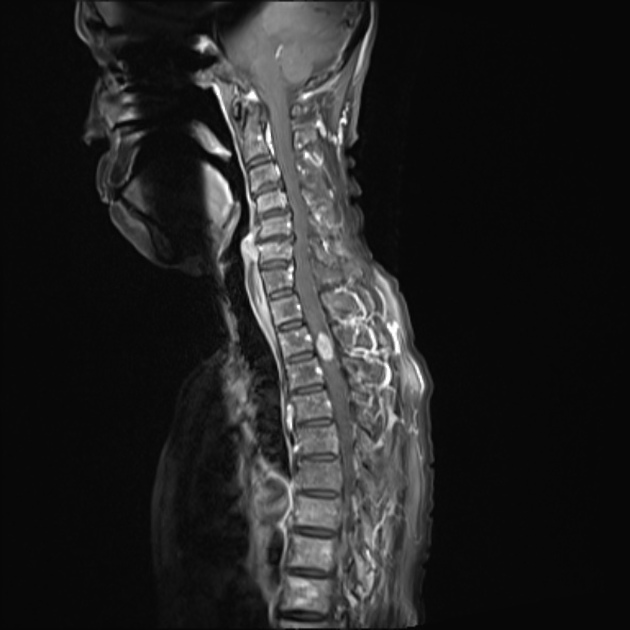
MRI
well-circumscribed
broad-based dural attachment
dural tail sign (60-70%)
ginkgo leaf sign in meningiomas arising lateral or ventrolateral to the spinal cord 14
They share similar signal characteristics to typical intracranial meningiomas:
T1: isointense to slightly hypointense, possibly heterogeneous
T2: isointense to slightly hyperintense
T1 C+ (Gd): moderate homogeneous enhancement
Occasionally, densely calcified meningiomas are hypointense on T1 and T2 and show only minimal contrast enhancement.
Treatment and prognosis
Spinal meningiomas are typically slow-growing. Surgery is the treatment of choice and complete tumour removal is achieved in the vast majority of patients. Less than 10% experience recurrence 2.
Differential diagnosis
The primary differential consists of nerve sheath tumours (spinal schwannoma and spinal neurofibroma), which may be differentiated by:
anterior location (meningiomas are usually located posterolaterally, except in the cervical spine 6)
tendency for multiplicity
low-intensity central regions on post-contrast T1 and T2 weighted images
neural exit foraminal widening (more common in nerve sheath tumours)
absence of a broad dural base

















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.