This is a basic article for medical students and other non-radiologists
Ischemic stroke is a clinical diagnosis where an acute neurological deficit follows brain infarction.
On this page:
Reference article
This is a summary article; read more in our article on ischemic stroke.
Summary
-
anatomy
-
epidemiology
-
common, accounts for 80% of stroke overall 1
the other 20% is hemorrhagic stroke
leading cause of disability
third highest cause of mortality in the UK 2,3
-
-
presentation
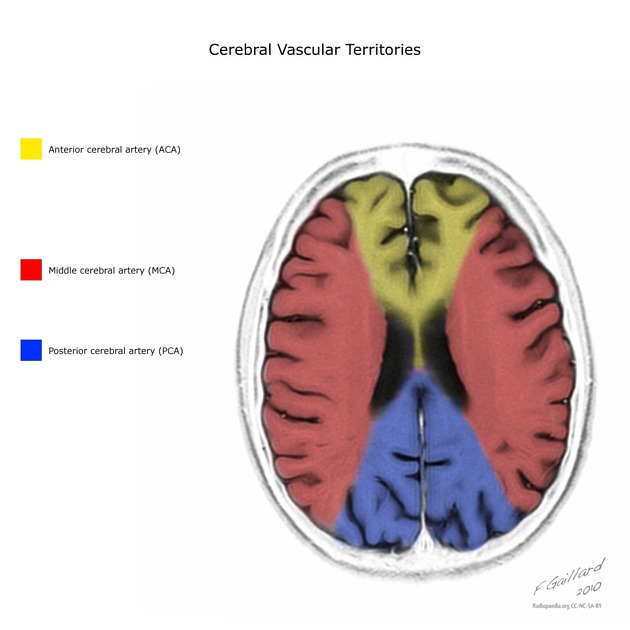
sudden focal neurological deficit whereby the exact clinical features depend on the specific vascular territory involved
time of onset is important when considering treatment
-
pathophysiology
brain parenchyma is deprived of blood flow and therefore oxygen, usually due to an artery being occluded by thrombus or embolus
cell death results in edema and swelling
common causes include atrial fibrillation, carotid artery stenosis, and cervical artery dissection
-
investigation
-
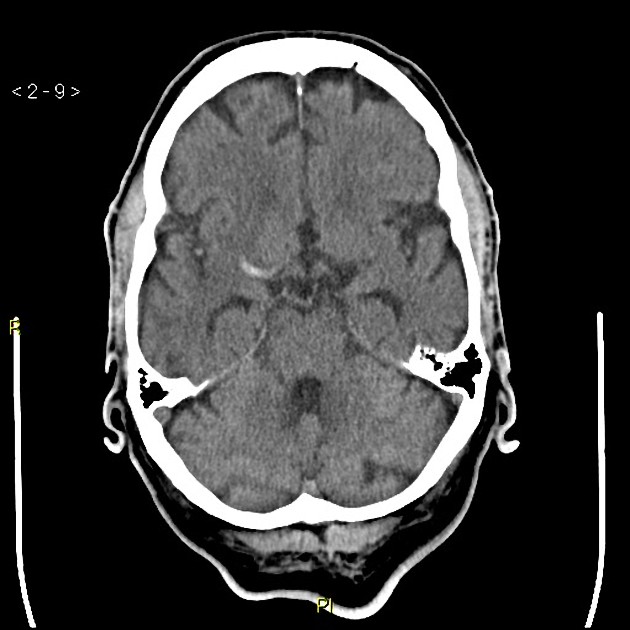
non-contrast CT head in the first instance
exclude hemorrhage or other cause
may show hyperdense vessel or evidence of infarction
-
CT angiography
used to identify the occluded artery
may identify the cause of the ischemic stroke, e.g. carotid stenosis, dissection, intracranial atherosclerotic disease
-
CT perfusion
used in some centers to identify infarcted brain ("core") and brain tissue at risk of infarcting ("penumbra")
-
MRI
less commonly used acutely in most centers, but is the best imaging modality for identifying infarcts (especially using the DWI sequence)
-
ultrasound
carotid Doppler ultrasound in the peri-stroke period to identify patients with carotid stenosis and then select patients who may benefit from endarterectomy
cardiac investigations are also performed to determine evidence of atrial fibrillation, which is an important cause of ischemic stroke
-
-
treatment
all patients with stroke should be managed in a dedicated stroke unit where possible, with input from the local stroke service
-
acute treatment
-
intravenous thrombolysis
for ischemic strokes <4.5 hours old, but can be given up to 9 hours or in wake-up situations in certain circumstances
depends on the local protocol
-
endovascular clot retrieval (mechanical thrombectomy)
for ischemic stroke due to large vessel occlusion
-
-
secondary prevention
oral antiplatelet therapy
statin
medical management of hypertension, diabetes mellitus, and other risk factors
Imaging
-
role of imaging
is there evidence of ischemic stroke?
what is the distribution and severity of the stroke?
is there hemorrhagic transformation?
is a cause visible, e.g. in situ thrombus?
are there contraindications to intravenous thrombolysis?
are there indications for endovascular clot retrieval?
is there significant carotid stenosis?
-
radiographic features
-
CT
parenchymal infarction may not be visible in the acute setting
with time, cytotoxic edema causes reduced density on CT
clot within a vessel may be seen as hyperdensity
acute hemorrhage will appear dense
-
MRI
the most important sequence is the DWI (diffusion sequence)
diffusion restriction in this context is highly sensitive for ischemia
-
angiography (CTA/MRA/DSA)
assessment of arterial supply to confirm whether a clot is present
-
perfusion (CT/MRI)
assessment of core and penumbra
-
carotid Doppler
not in the acute setting but usually within two weeks following stroke
assessment of the neck vessels looking for carotid stenosis
if >70% stenosis on affected side, surgery may be offered
-










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.